This is a question that you will have asked more than once all of you who are performing this technique:)
As we have commented in other posts, punch grafts, even if they do not adhere to the wound bed, release growth factors and cells that, in addition to promoting healing, also reduce pain. (See post: “Punch grafting as a painkiller for painful ulcers“) That is why its list of “unofficial” indications is so extensive and can include arterial ulcers that are not candidates for revascularization, when the patient does not want amputation.
So, taking into account the wide profile of ulcers that we can treat with punch grafting, we must be open-minded when evaluating success or failure. What we should never graft are infected wounds or ulcers in which we have not optimized the etiological treatment.
We speak of attachment when, at the first dressing change from the 4th day of the procedure (ideally, one week later), the grafts are adhered to the bed and present a pink-bluish coloration, a sign that neoangiogenesis (formation of new vessels that nourish the dermis and epidermis) has occurred.
Well, this ideal attachment in the first week occurs when we graft a bed in optimal conditions … That is, rarely … Not to say almost never … 😉 Therefore, it is normal in clinical practice that, especially when grafting wounds with some slough (usually it is not possible to achieve an optimal bed), we find grafts with yellowish or whitish coloration that remain in the bed by imbibition. In this situation we will not do any type of cleaning on the bed and we will make a new cure a week later (if the exudate allows it). In the following dressing changes some grafts, or even all of them, may become detached 🙂


I would like to underline that in a study we conducted on venous ulcers, compressive therapy and punch grafts, ulcers with a percentage of sloughy tissue in their bed greater than 50% showed no less tendency to complete epithelialization:)
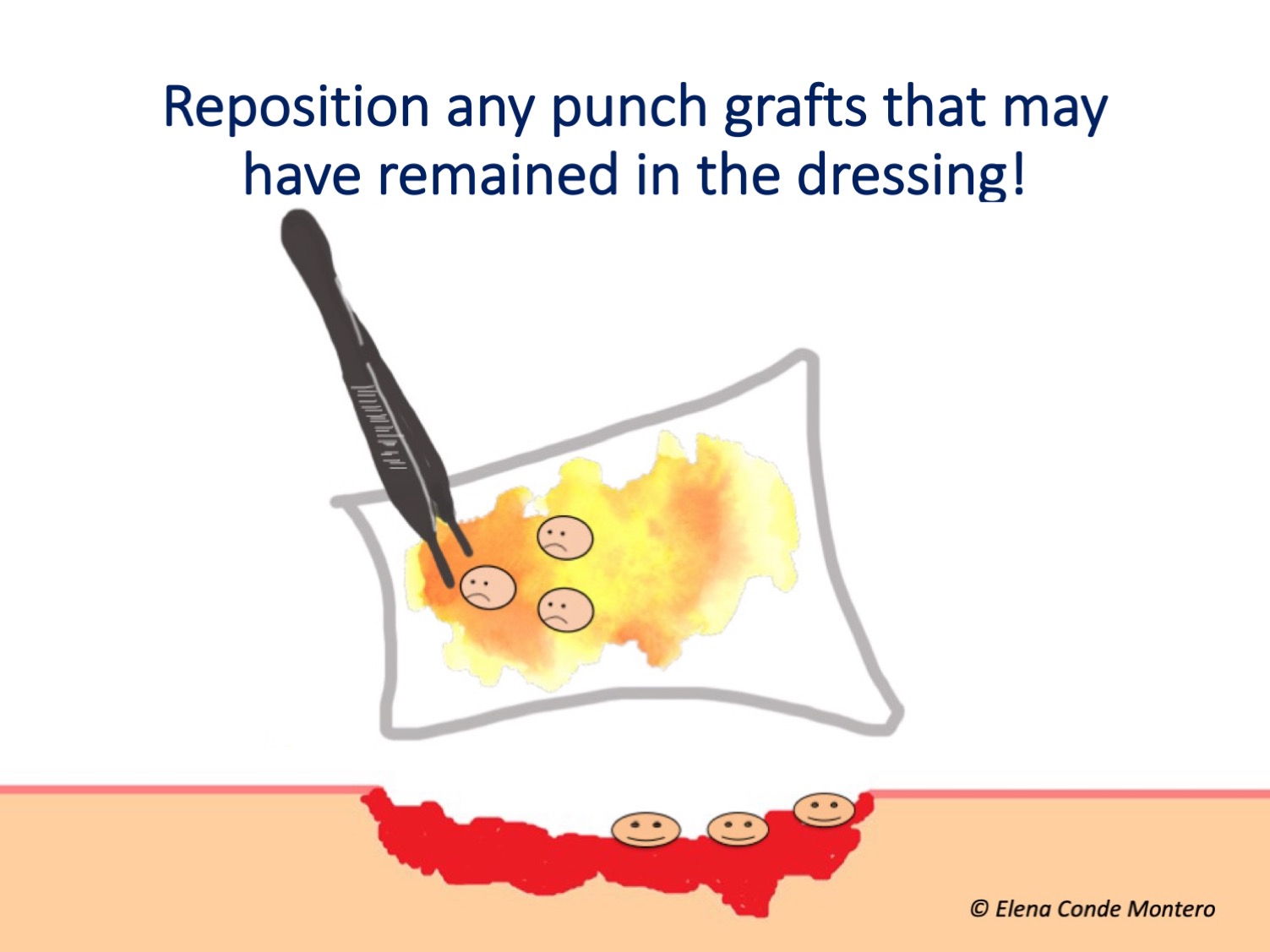
– And what do I do if from the first dressings there is no data of attachment and many of the grafts remain in the dressing?
The first thing you should do is to reposition in the wound the grafts that have remained in the dressing (See post: “Repositioning and not removing the scabs: two unwritten rules of punch grafting“). Speaking of dressing… There are no comparative studies on the usefulness of different dressings in the grafted area.
- Secondly, in lower limb wounds, you should ask the patient and family members if they have been on absolute bed rest. Absolute bed rest with the legs elevated, at least the first 4 days (although we always recommend a minimum of one week), is essential to promote graft attachment in lower limb wounds. In fact, this is the main cause of graft failure in our practice, which forces us to admit those patients who cannot perform adequate rest at home.
- Thirdly, reconsider whether the problem may have been inadequate bed preparation prior to coverage. Before the next coverage, make sure to minimize the presence of biofilm.
- In case we find complicated locations, such as the Achilles tendon or the malleolus, or beds with a lot of slough that we cannot remove or very undermined, we have to think that what may have failed is insufficient contact and pressure of the grafts with the wound, so the next coverage with grafts would be performed with ambulatory negative pressure therapy (See post: “Punch grafting and negative pressure therapy: a successful couple“).

- If you have grafted an ulcer in the spectrum of arteriolosclerosis, for example, a Martorell ulcer, early, with active necrosis and abundant slough, think that your objective was not to achieve attachment with those first grafts, but a reduction of pain, control of necrosis and improvement of the bed for the following coverings. Sequential grafts every 3 weeks or so will help us to achieve complete epithelialization in these cases (see post: “How to close large ulcers after minor trauma in the elderly“).
- Finally, rethink the diagnosis of ulcers that, despite having been grafted in near-optimal conditions and with adequate etiological treatment, do not respond.
– And what has gone wrong when punch grafts take hold but in the following weeks are lost?
This usually happens in venous ulcers of long evolution. Resting with the legs elevated controls venous hypertension, but this is lost when the person begins to lead a normal life because, in spite of using compressive therapy, he does not take anti-edema measures, such as having the legs elevated during rest. A sign of venous congestion associated with venous hypertension is the maroon-purple color of these grafts prior to their detachment. It is essential to insist on the importance of anti-edema measures in people with venous ulcers!

– And when the problem is that, despite adequate compression and rest, in the successive dressing changes during the first weeks we do not get a complete epithelialization, with excessive exudate?
As I commented in the post “In which situations would it be better to remove the bandage and leave the legs elevated and open air?“, the problem in this case is occlusion. Therefore, the solution is to remove the dressings and bandages and leave the legs open air. To control edema in parallel, it is essential to rest with the legs elevated. Our experience is very good with the application of zinc oxide drying solution once or twice a day. To perform this strategy we usually need a hospital admission.

Have you already performed punch grafting? What is your experience?
Also available in: Español (Spanish)






