Heart failure is the most frequent reason for hospitalization and readmission in the elderly. Although we do not usually think of it as a potential trigger for leg wounds, the reality is that it is a frequent cause of the appearance or worsening of leg ulcers. I am sure that reading this will have brought to your mind a case from the practice 😉
Why may heart failure trigger leg wounds?
Peripheral edema is a typical sign of congestive heart failure and, in episodes of decompensation, this edema can develop rapidly.
It is a bilateral edema, which often appears in combination with obesity, phlebolymphedema or hypoalbuminemia.
This edema may be related to left and/or right heart failure, to the autoregulation mechanisms of the cardiovascular system, as well as to concomitant fluid retention and/or to the medication used to treat it. In patients with right heart failure, blood stasis occurs, with swelling and accumulation of peripheral fluid. In left-sided heart failure, the increase in cardiac output, in addition to the possible influence on the deterioration of right-sided cardiac function, also activates compensatory mechanisms (nervous and hormonal) that result in peripheral edema related to the action of the renin-angiotensin system and sodium and water retention.
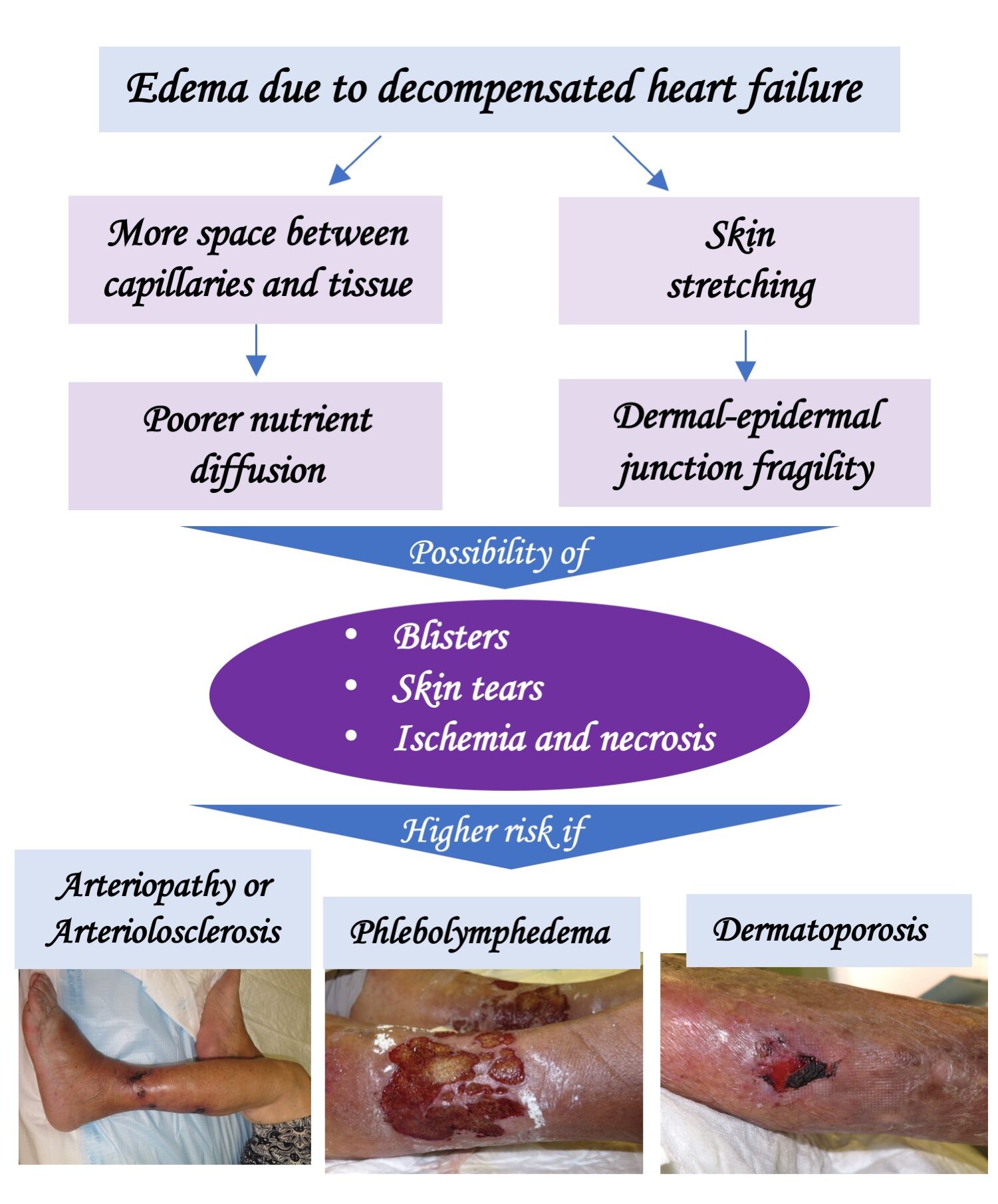
Whenever there is edema in the legs, regardless of its cause, the space between the capillaries and the tissue increases. This leads to poorer diffusion of nutrients and, as a consequence, decreased skin perfusion. Therefore, especially in patients with arterio/arteriolosclerosis or phlebolymphedema, in whom perfusion is already deficient at baseline, perfusion may become insufficient and cutaneous ischemia and necrosis may develop. In fact, it is not uncommon for Martorell ulcers (ulcers due to subcutaneous ischemic arteriolosclerosis) or arterial ulcers to develop after an episode of decompensated heart failure. On the other hand, heart failure is considered to be a risk factor for venous ulceration.2
In addition, fluid accumulation in the legs involves skin stretching and the possibility of detachment at the dermoepidermal junction, with the appearance of fissures, erosions and/or blisters. The condition will be more severe in people with dermatoporosis (see post: “Wounds secondary to dermatoporosis or chronic cutaneous insufficiency”), in whom skin tears will easily appear.
Bearing in mind that heart failure is a syndrome typical of the elderly, it is not uncommon for the same person to present together a certain degree of arterio/arteriolopathy, chronic venous and lymphatic insufficiency and dermatoporosis, which increases the risk of ulcers with a torpid evolution.
How should these wounds be managed?
The essential thing is to correct the cause of the edema, that is, to control heart failure, with diuretics and other drugs, for which the role of the internist is fundamental (I feel very fortunate to work surrounded by internists).
In order to be a pillar in the treatment of these ulcers, it is important that the diagnosis includes heart failure as a precipitating factor. For example: “Martorell ulcer in the context of an episode of decompensated heart failure”.
After correction of cardiac decompensation, compression therapy adapted to the needs and tolerance of each individual (provided there is no severe peripheral artery disease) will be of beneficial,1,3 starting with low pressures and devices with low resting pressure (short-stretch bandages, multicomponent systems, self-adjusting wraps with Velcro-type closure). Of course, anti-edema measures (rest with legs elevated) and muscle activation with dorsiflexion and plantar flexion exercises are also fundamental, even in patients with reduced mobility (See post: “What exercises can I do at home against phlebolymphedema?”) These measures are also important in a preventive manner, associated with adequate follow-up and control of heart failure. Taking into account that these people are usually elderly, with phlebolymphedema and/or skin fragility, we will preferably recommend skin protection socks and self-adjusting compression wraps (“Why are adjustable compression wrap devices so popular?”).

As discussed in the post “New recommendations about compression therapy“, it is recommended not to apply compression in severe cases of heart failure (NYHA IV = inability to perform any physical activity without discomfort, with symptoms even at rest). In less severe cases, the progressive increase in compression produces only very short phases of increased cardiac load and can facilitate a substantial reduction in peripheral edema.1
Depending on the comorbidities and underlying etiology, we may consider strategies that accelerate healing, such as negative pressure therapy or punch grafting.
A final thought: “How many people are suffering from leg wounds with poor evolution due to inadequate control of heart failure?
References:
- Urbanek, T., Juśko, M., & Kuczmik, W. (2020). Compression therapy for leg oedema in patients with heart failure. ESC Heart Failure, 7, 2012 – 2020.
- Augey F, Pinet A, Renaudier P. Insuffisance cardiaque et ulcère de stase : une association significative (étude prospective de 100 cas) [Heart failure and stasis ulcer: A significant association (prospective study of 100 cases)]. Ann Dermatol Venereol. 2010 May;137(5):353-8.
- Saucedo D, Evans N, Lim CS. Initiating compression therapy for those living with heart failure. Br J Community Nurs. 2021 Sep 1;26(Sup9):S12-S17.
Also available in: Español (Spanish)