Because it does not include information that is very relevant in the evaluation of these wounds…
As a reminder, the most widespread and widely used classification of pressure ulcers is the NPUAP/EPUAP (National/European Pressure Ulcer Advisory Panel) system, which only includes the depth of the wound.
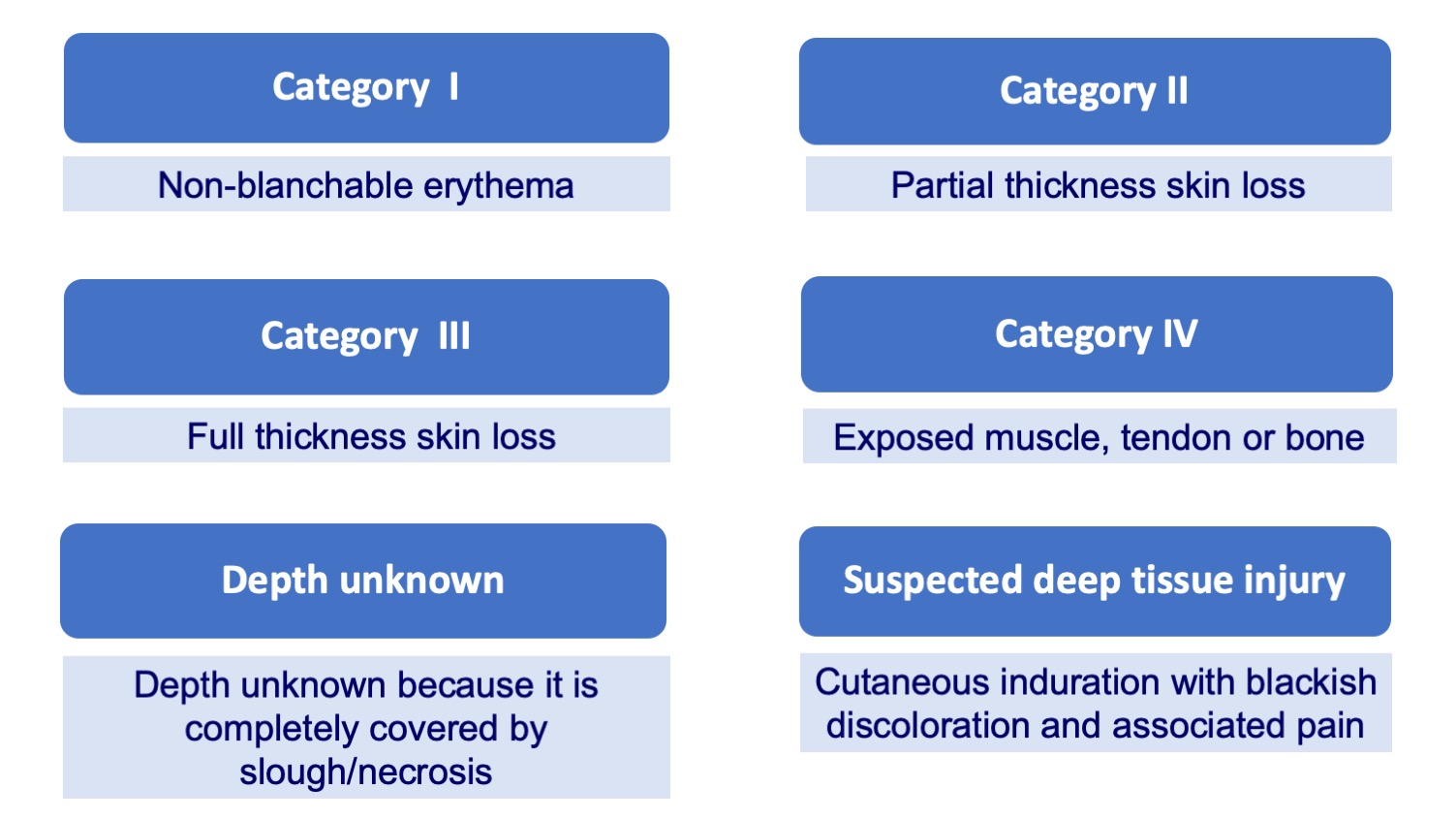
The problem is that talking only about the depth does not give us enough information to get an idea of the prognosis and decide the best treatment in each case… In fact, many times, the main conditioner of the evolution is ischemia or osteomyelitis, which are not recorded in this classification (See post “Do not debride dry eschars on heels“). And, of course, the general condition and baseline situation of the person.
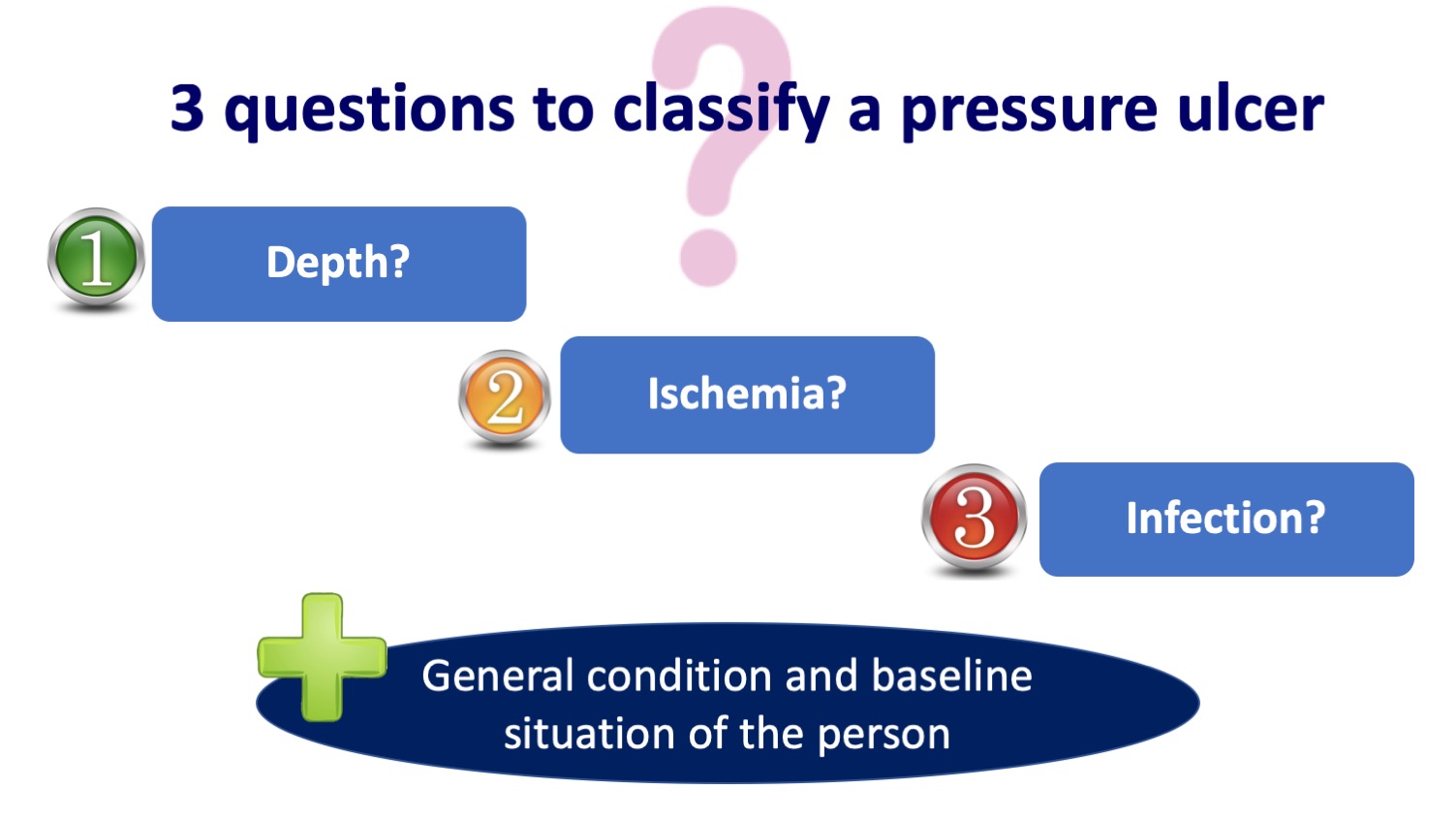
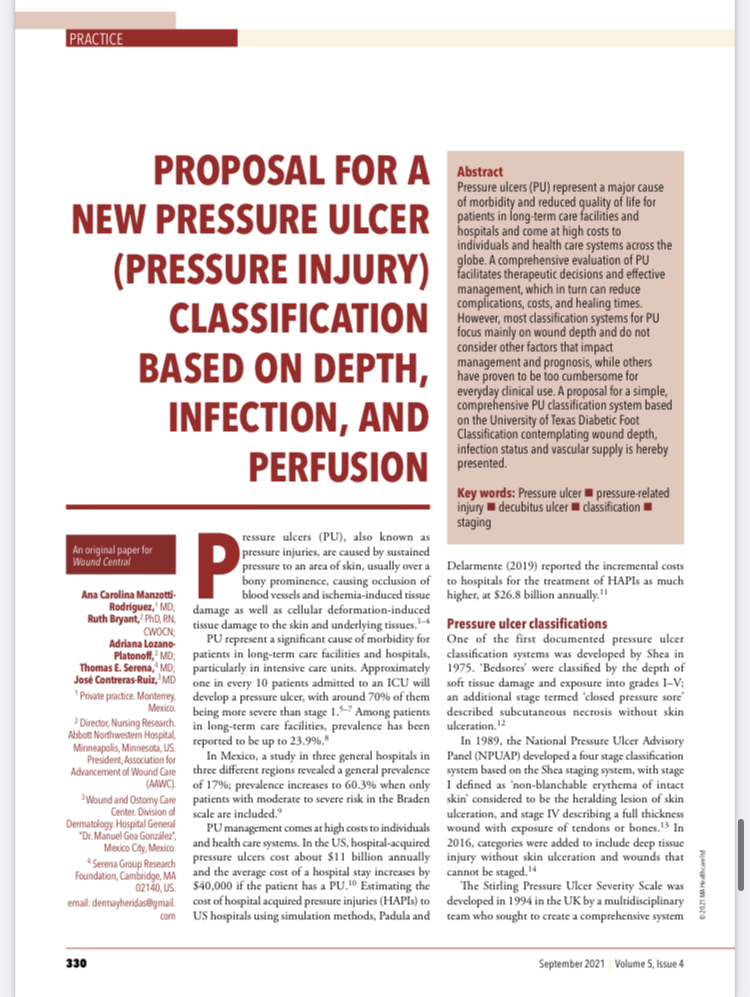
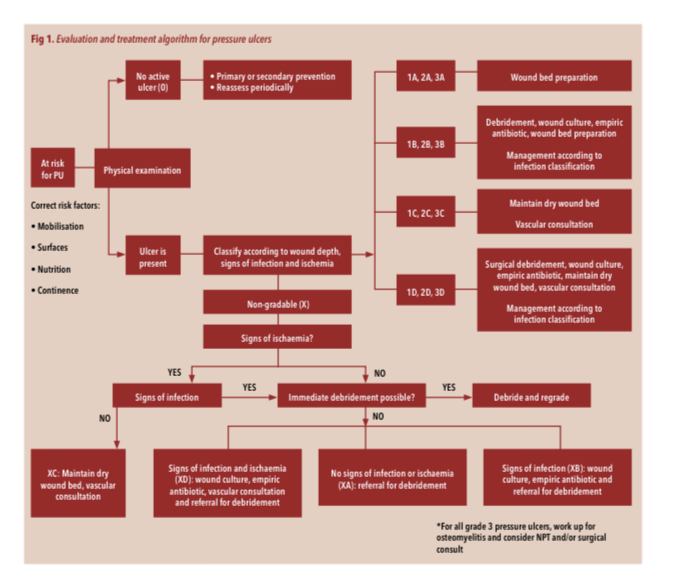
Although I had already reflected many times on the limitations of this classification, I have been encouraged to write on the subject after reading two articles that have just been published by the working group of my friend and great expert in wounds, José Contreras, which you will find at the end of this entry. These authors propose a new classification of pressure ulcers including, in addition to depth, ischemia and infection. This classification is called DIP (Depth, Infection, Perfusion) and is inspired by the University of Texas diabetic foot lesion classification scale.
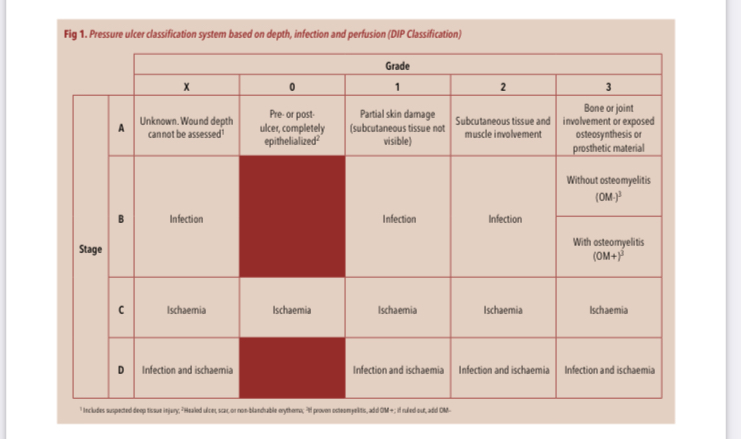
What are the most relevant practical aspects of this new DIP classification proposal?
- Grade 0 represents a pre- or postulcerous lesion that includes healed ulcers, scars and non-blanching erythema. Although this grade does not describe a true ulcer, it helps identify sites at high risk for ulceration or re-ulceration.
- Wounds with bone or joint involvement are included in a specific category (grade III), as they have a worse prognosis.
- Grade III ulcers have a high risk of osteomyelitis, so this should be ruled out if the evolution is not favorable.
- It is mandatory to palpate pulses in any person with a heel pressure ulcer.
- The presence of ischemia, regardless of the depth of the ulcer, will require an assessment by vascular surgery.
- In case of ischemia and absence of infection, debridement should be avoided and the wound kept dry if there is no possibility of revascularization. On the contrary, if there is ischemia and signs of infection, it is essential to remove the non-viable tissue to control the infection.
Finally, I would like to stress that, although the characteristics of the ulcer will establish the treatment to be followed and are a prognostic marker, the mobility, mental state and general condition of the person are a fundamental pillar in decision making. In people at the end of life, the most important thing is to seek wellbeing, spacing the cures as much as possible without being invasive. In fact, this strategy of touching wounds as little as possible is the strategy of choice in Kennedy’s so-called terminal ulcers. Although their exact etiology is unknown, these rapidly progressive multiple pressure ulcers could be framed as multi-organ failure.
Also available in: Español (Spanish)






