The CEAP classification (Clinical-Etiological-Anatomical-Pathophysiological) was created in 1994 to standardize the diverse manifestations of chronic venous disease. It was modified in 2004 to refer more broadly to chronic venous disorders. Therefore, it covers the broad spectrum of morphological and functional alterations of the venous system.
It is interesting to differentiate these terms, which have been defined by international consensus:
Chronic venous disorders: it includes the whole spectrum of morphological and functional anomalies of the venous system.
Chronic venous disease: used when the morphological or functional alterations (valvular incompetence) are present of long duration and manifested with signs and symptoms that need to be studied and treated. Valvular incompetence is identified with duplex ultrasound as a retrograde venous flow of prolonged duration. Symptoms include pain, burning, itching, heaviness, fatigue, muscle cramps. Signs include dilated veins (telangiectasias, varicose veins), oedema, skin alterations and ulceration. The severity of signs and symptoms does not always correlate with the degree of underlying valve dysfunction.
Chronic venous insufficiency: used for patients with chronic venous disease who present clinical signs of greater involvement, such as significant oedema, skin changes, or ulceration.
As its name indicates, the CEAP classification is composed of 4 sub-classifications:
C: Clinical
E: Etiological
A: Anatomical
P: Pathophysiological
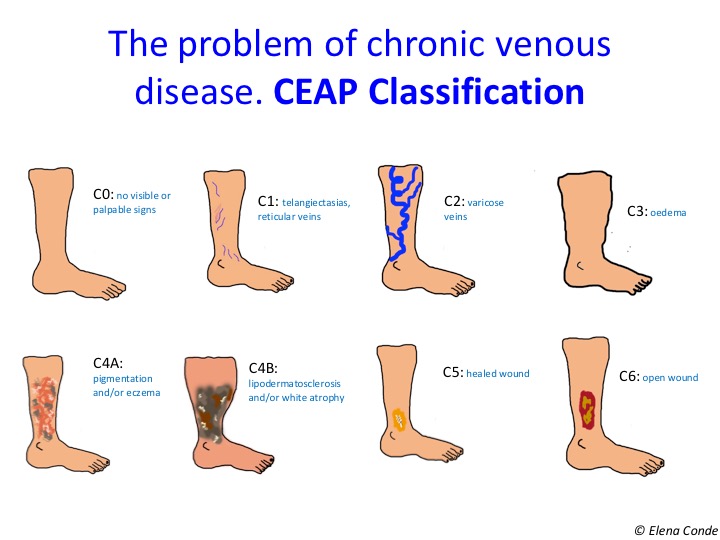
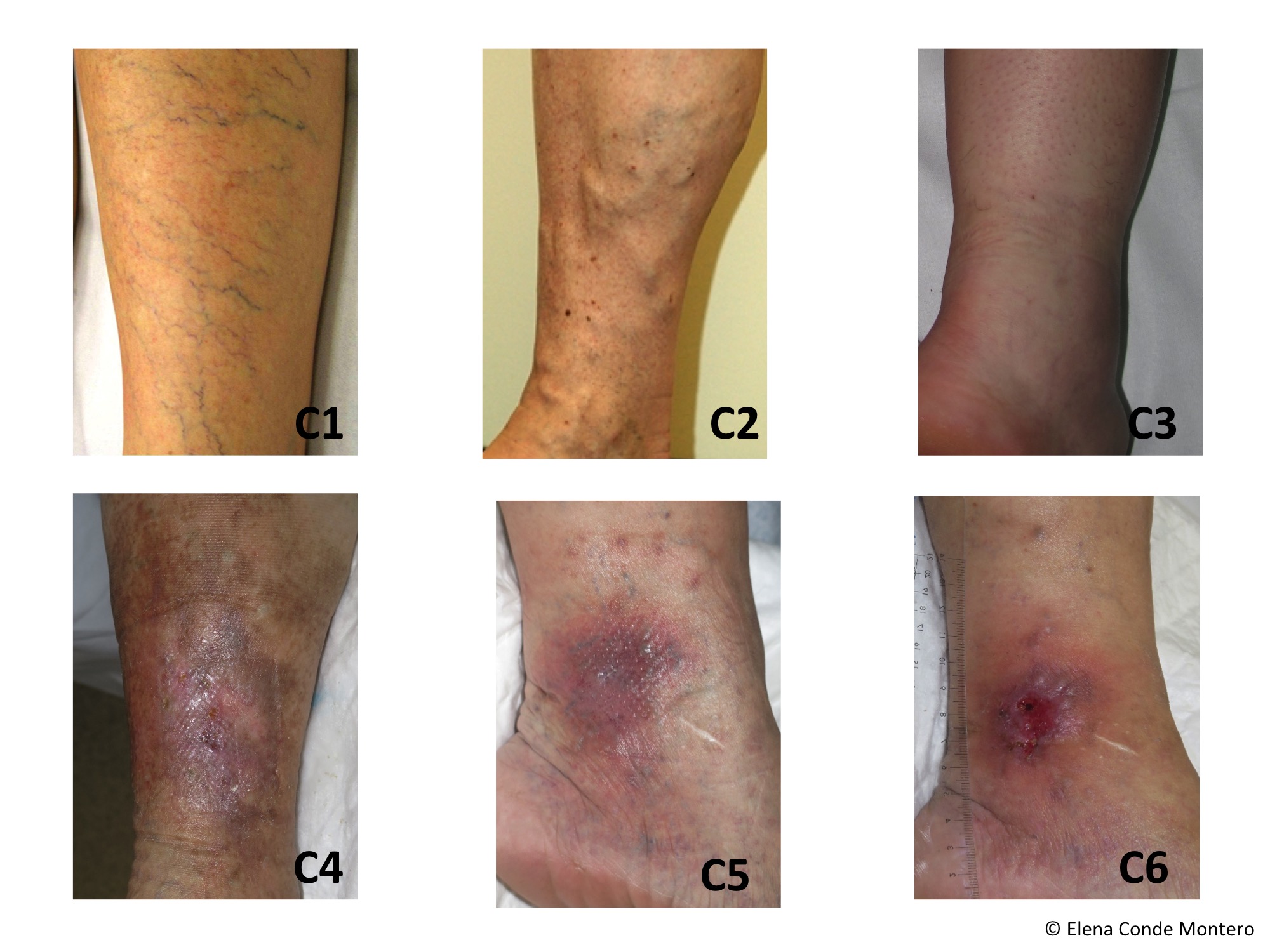
C (Clinical): We often use it in isolation.
- C0: no visible or palpable signs
- C1: telangiectasias (veins less than <1mm), reticular veins (1-3 mm in diameter)
- C2: varicose veins (>3mm)
- C3: oedema
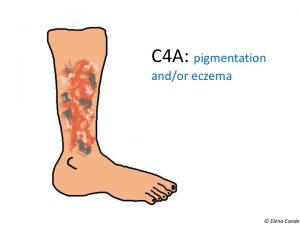
- C4: secondary skin alterations
- C4a: pigmentation, eczema, or both
- Pigmentation is a brown-greyish coloration of the skin due to hemosiderin deposition by extravasation of red blood cells. It usually occurs in the ankle, but can affect the foot and rest of the leg.
- Eczema is an erythematous and desquamative dermatitis, which can develop vesicles and exudate.
- C4a: pigmentation, eczema, or both
-
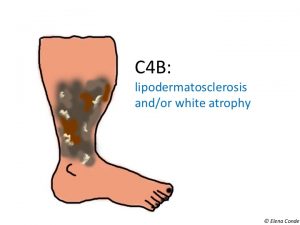
- C4b: lipodermatosclerosis, white atrophy, or both
-
-
- Lipodermatosclerosis is the result of oedema and chronic inflammation, with consequent thickening and fibrosis of the skin and subcutaneous cellular tissue.
- White atrophy (Atrophie blanche) is a circular or starred area of scar-like appearance, depressed, with pearly-white coloration, surrounded by dilated capillaries and hyperpigmentation.
-
- C5: healed ulcer
- C6: open ulcer (often in the ankle area
The C classification is completed with the presence or absence of symptoms (pain, itching, heavy legs, cramps, others):
- A: asymptomatic
- B: symptomatic
E (Etiological)
- Ep: primary (develops independently of other diseases)
- Ec: congenital (present at birth or developing in infancy)
- Es: secondary, if it appears as a consequence of another disorder, such as trauma or thrombosis (post-thrombotic syndrome)
- En: absence of identified venous aetiology
A (Anatomical): The venous system consists of a superficial venous system and a deep venous system. The veins that join vessels within the same system are called communicating veins, while those that connect the superficial to the deep ones are called perforating veins. In order to identify the exact location of the venous anomaly, the venous system has been divided into 18 anatomical segments within the general classification of superficial (As), deep (AD) and perforating (AP) veins. Sometimes the affected segment (An) cannot be determined.
If you want to know more about the anatomy of the venous system of the lower limb: Meissner MH (2005) Lower extremity venous anatomy.
- AS1-5: superficial venous system
- As1: telangiectasias or reticular veins
- As2: great saphenous vein above the knee
- As3: great saphenous vein below the knee
- As4: small saphenous vein
- As5: non-saphenous vein
- AD6-16: deep venous system (D= Deep)
- AD6: inferior vena cava
- AD7: common iliac vein
- AD8: internal iliac vein
- AD9 : external iliac vein
- AD10: pelvic
- AD11: common femoral vein
- AD12: deep femoral vein
- AD13: femoral vein
- AD14: popliteal vein
- AD15: anterior tibial, posterior tibial, peroneal veins
- AD16: muscular (gastrocnemius, soleus)
- Ap17-18:perforating veins
- Ap17: thigh
- Ap18: twin
- An: unidentified anatomical location
P (Pathophysiology): indicates the presence of venous reflux or obstruction.
The venous blood flow is determined by the drainage from the superficial to the deep system, thanks to the muscular contraction that overcomes gravity, and to the prevention of its reflux by the closing of the venous valves.
- PR: Reflux
Valvular alterations, congenital or secondary (trauma, thrombosis), can produce different degrees of retrograde flow (abnormal if it lasts more than 0.5 seconds, detected by duplex ultrasound). Deep reflux is usually associated with more severe clinical symptoms. However, ulcer occurrence with isolated superficial venous reflux is also possible.
- PO: Obstruction
Superficial and deep venous thrombosis cause an obstruction that hinders venous flow. Consequently, superficial veins become tortuous and alternative drainage routes are developed. Although the thrombus may be partially or totally reabsorbed, damage to the wall segment and valves is permanent.
- PR,O: reflux/obstruction
- Pn: unidentified venous pathophysiology
References:
- Eklöf B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, Meissner MH, Moneta GL, Myers K, Padberg FT, Perrin M, Ruckley CV, Smith PC, Wakefield TW. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(6):1248
- Eklof B, Perrin M, Delis KT, Rutherford RB, Gloviczki P. Updated terminology of chronic venous disorders: the VEIN-TERM transatlantic interdisciplinary consensus document. J Vasc Surg. 2009;49(2):498
- Moneta G. Classification of lower extremity chronic venous disorders. UpToDate, last updated august 2014
- Meissner MH (2005) Lower extremity venous anatomy. Semin Intervent Radiol. 2005 ; 22: 147–156.
Also available in: Español (Spanish)




Elena,
Hi,
I am a Physical therapist active in wound care. I speak regularly in the US. I am giving a talk on the CEAP classification and its realtionship to lymphedema.
I do love your picutres. I am wondering if I could use some of them for a talk. What is the process to do so?
Dear Marta,
Thank you for your message! Of course, you can use any pictures you may need:)