In our daily life as a health care professional treating patients with leg ulcers, have you ever used or heard the word PHLEBOLYMPHEDEMA? Probably rarely or never… But you have certainly seen and treated patients with legs very similar to the ones you can see below:


What name do you use then to refer to the aetiology of these very frequent skin changes in the legs? I’m sure the range of answers is very wide, but the words LYMPHEDEMA or CHRONIC VENOUS INSUFFICIENCY will predominate. The use of this varied terminology clearly indicates that we do not call PHLEBOLYMPHEDEMA by its name.
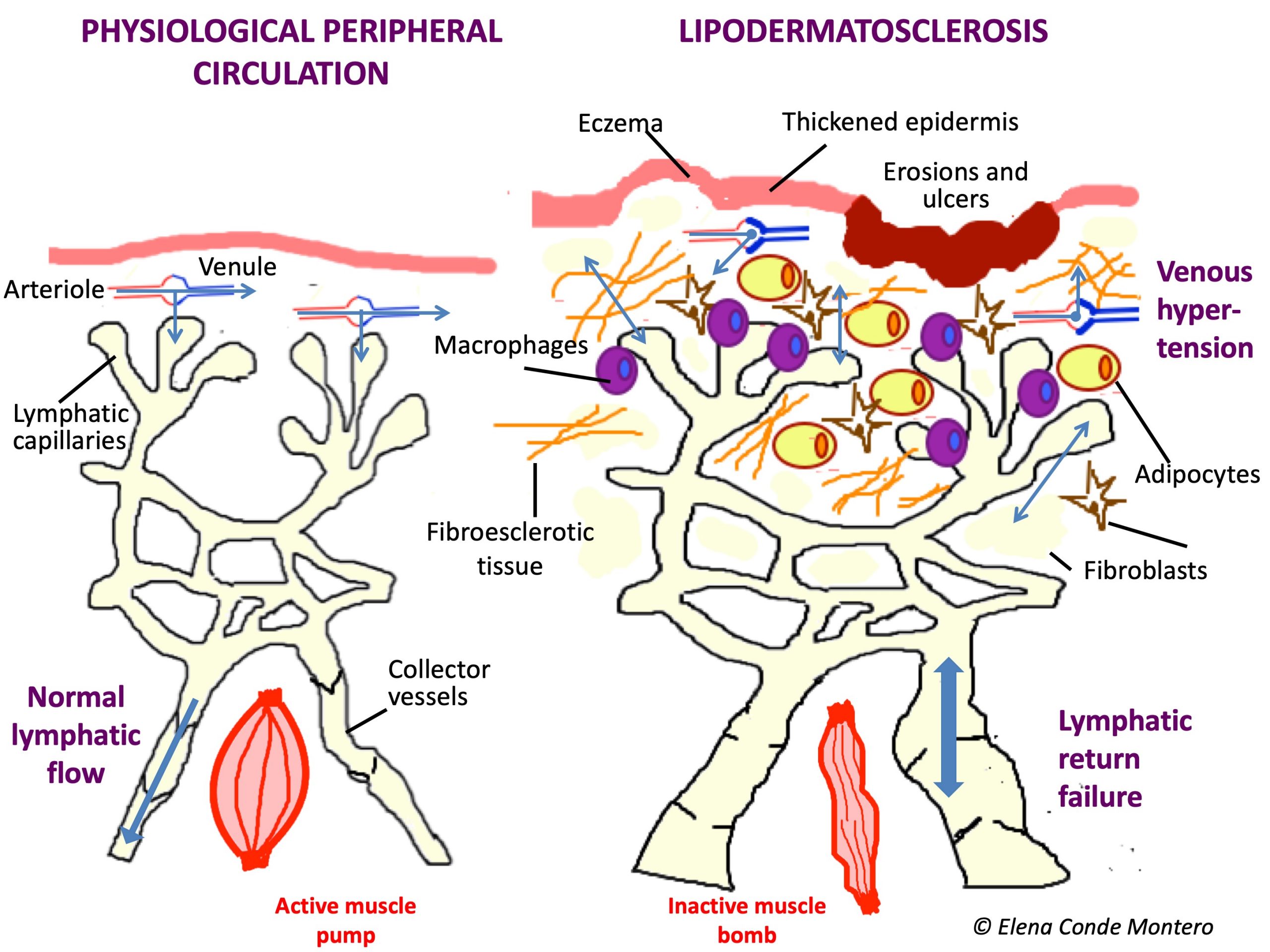
Why don´t we usually use this term, when it is the most frequent cause of lymphedema in our environment and it is very common in our consultations? The reason is undoubtedly a lack of knowledge of physiopathology. We are not clear about what is happening in the microcirculation of those swollen legs because our mind has not internalized that uncontrolled venous hypertension will end up generating a collapse and damage of the lymphatic capillaries and that, therefore, the venous edema will become venous and lymphatic. In fact, that edema, with episodes of lesser or greater redness and progressive appearance of woody consistency, warty lesions, erosions or ulcers, and possibility of superinfection, is the result of venous insufficiency and secondary lymphatic insufficiency.


In addition, possible co-morbidities of these patients, such as congestive heart failure, cirrhosis or nephropathy, may obstruct lymphatic drainage of interstitial fluid and macromolecules.
Most of our patients with phlebolymphedema have mobilization problems, especially osteoarticular ones. This lack of activation of the muscle pump not only influences the venous return, but also the lymphatic return, since the walls of the lymphatics also need muscle contraction to overcome gravity.
Therefore, although at an academic level it is simpler to explain and study the causes of leg edema in separated compartments, in clinical practice we very often find combined aetiologies. The detection of all the factors that may be involved in the edema development is fundamental to carry out an adequate and early treatment. I want to emphasize “early” because uncontrolled edema, with the presence of proteins and other molecules in the interstitium, produces a pro-inflammatory environment that produces fibrosis in the subcutaneous cellular tissue and the vessel wall, with irreversible damage, in addition to promoting bacterial proliferation with cellulitis risk. In order to stop this lipodermatosclerosis as soon as possible, it is essential to quickly reduce the edema and maintain it over time.
Undoubtedly, using terms that take into account the different aetiologies involved, such as PHLEBOLYMPHEDEMA, means that we are very aware from the outset of the targets of our treatment.
The diagnosis of phlebolymphedema is clinical (with great importance of anamnesis), but we can also help us with imaging tests such as echo-Doppler and lymphoscintigraphy. It is characterized by signs of chronic venous insufficiency, such as phlebectasic crown in the foot or ochre coloration secondary to hemosiderin deposits, signs of lymphatic insufficiency, such as edema on the back of the feet and toes, and changes in epidermis, dermis and subcutaneous cellular tissue associated with chronic edema, such as eczema, vesicles or warty lesions (variability depending on chronicity), and the fibrous consistency typical of lipodermatosclerosis.



It is often bilateral, but usually one leg is more affected than the other. Note: a frequent differential diagnosis presented by these legs is cellulitis. However, even though the risk of infection in these patients is higher, the development of cellulitis would be only in one leg. So, even though these legs sometimes appear very red, swollen and hot… We would never suspect a bilateral cellulitis!
The idea of talking about phlebolymphedema just came to me in Zurich, at the annual meeting of the European Venous Forum. At this congress, the relevance of the alteration of the microcirculation of the lymphatic capillaries associated with venous hypertension was repeatedly discussed. Consequently, I thought about the scarce use the word PHLEBOLYMPHEDEMA, when it is the most appropriate term in many of our patients. In this meeting I also thought about another term: LIPEDEMA. I totally agree with the experts who, taking into account that the presence of edema in lipedema has not been demonstrated, propose that it would be more purist to talk about PAINFUL LIPOPHYPERTROPHY. But since the term is established, we will probably continue to talk about LIPEDEMA… So we will continue to talk inadequately…
The “wrongly named” lipedema sometimes also overlaps with phlebolymphedema and we would talk about PHLEBOLIPOLYMPHEDEMA. Furthermore, even if the typical clinical characteristics of lipedema are not met, it is not uncommon to find fat accumulation in the legs of these patients. This is because the chronic inflammation associated with phlebolymphedema not only produces fibrosis, but also stimulates the proliferation of adipocytes… A perfect vicious circle that must be cut as soon as possible, because in addition to facilitating ulcers, it also increases the risk of infection.
And regarding infections, it should also be noted that the proper functioning of the lymphatic system is an essential pillar of the immune system. Each episode of cellulitis in these legs with phlebolymphedema produces irreparable damage to the lymphatics, with the consequent development of recurrent infections.
CONCLUSION: there are many reasons that support the need for rapid treatment aimed at controlling venous and lymphatic insufficiency. In this management it is very important that different professionals collaborate, since the patient is going to benefit enormously from a multidisciplinary management in which the following list should be considered:
-
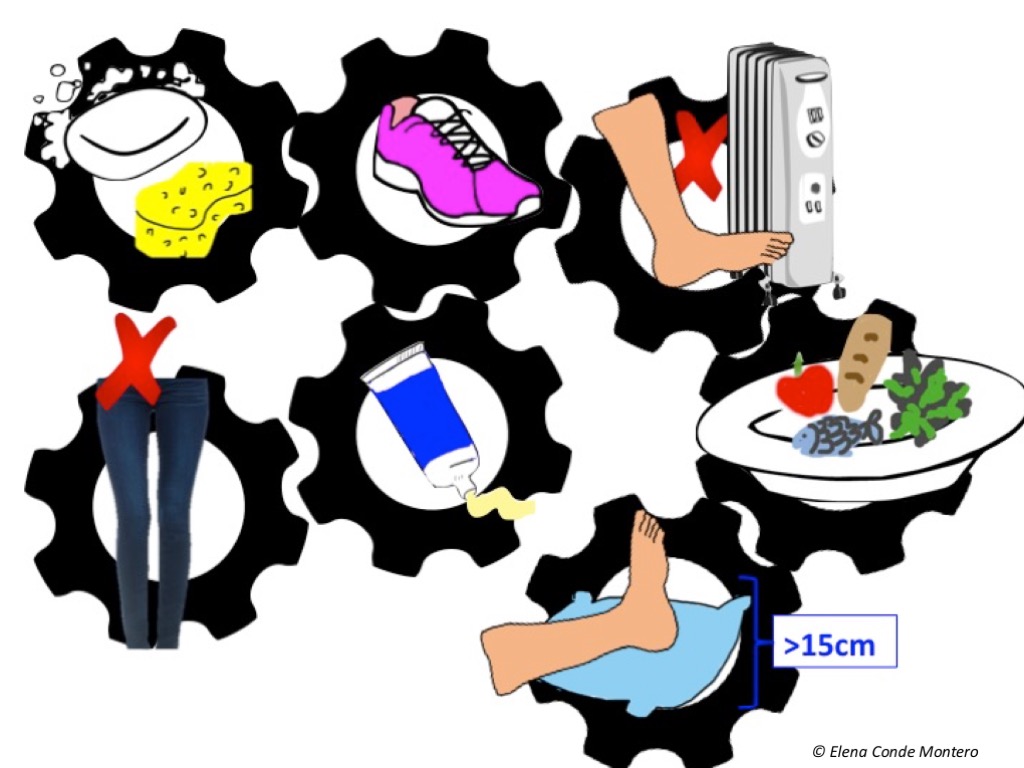
Skin hydratation and adequate hygiene
We must recommend cleaning and drying avoiding aggressive rubbing on the epidermis and that emollients are used daily. Patients must be informed of the risk of cellulitis, so they can consult if alarm signs appear (erythema, increased pain, fever). Multiple erosions and superficial ulcers in the context of hypodermitis respond very well to treatment with topical steroids and optimization of compressive therapy. The application of zinc oxide products will have a beneficial anti-inflammatory effect in the presence or not of cutaneous wounds in these legs (see post: “Why do we use topical zinc on wounds and perilesional skin?”) In case of developing ulcers of greater extension and depth, besides optimizing the local treatment, it is essential to ensure that the etiological treatment is adequate (mainly compression therapy).


-
Change of daily habits
We must emphasize compliance with anti-edema measures and provide professional help to achieve weight loss.
-
Sclerotherapy or other endovenous techniques
These techniques will be performed if, after an adequate ultrasound study, the detected reflux could benefit from this treatment (see post: “Sclerotherapy in venous ulcers: the sooner the better”). Unlike surgery, these are safe techniques to avoid damage to the lymphatic vessels. This correction of venous reflux, and therefore of venous hypertension, will have a direct impact on lymphatic insufficiency, which can be greatly improved.
-
Therapeutic compression
Bandages with a high static stiffness index (see post: “Band and bandage, not the same thing”) are the most indicated in these patients to try to reduce edema as soon as possible. After an initial intensive treatment with bandages, until the greatest possible reduction in the leg perimeters is achieved, maintenance treatment with compression stockings is usually recommended. The more advanced the phlebolymphedema, it will be preferable to use flat-knit stockings, since they have less stretching capacity than circular tissue and are custom-made, which makes them safer and more effective in these patients. Since the recommended pressure in these patients is high (30-40 mmHg) and they have difficulty putting on the stockings, self-adjustable velcro wraps are an effective alternative, easy to put on, and very well accepted by patients, families and caregivers.
-
Manual lymphatic drainage
With the hands, through very soft and slow movements, you can stimulate the lymphatic vessels to help them open and promote the drainage of the fluid from the areas with more congestion towards the proximal functional lymphatics
-
Physical exercise
Exercises that stimulate the calf and plantar muscle pump, which facilitate venous and lymphatic return, and therefore decrease venous hypertension and improve distal perfusion, are essential. The simple dorsiflexion movement of the foot and ankle is beneficial in those patients with reduced mobility. But if there is any “specially beneficial activity” that we should recommend without doubt is aquagym. Aquatic exercises are beneficial, not only because of the movement performed, but also because of the cold and pressure exerted, with an analgesic effect. ?

References:
- Farrow W. Phlebolymphedema-a common underdiagnosed and undertreated problem in the wound care clinic. J Am Col Certif Wound Spec. 2010 Apr 22;2(1):14-23.
- Bunke N, Brown K, Bergan J. Phlebolymphemeda: usually unrecognized, often poorly treated. Perspect Vasc Surg Endovasc Ther. 2009 Jun;21(2):65-8.
Also available in: Español (Spanish)






