Zinc in wounds is a subject that has never lost its relevance.
Zinc is a trace element, i.e. a metal found in the body in very small amounts, but it is essential for the activity of different enzymes and transcription factors (proteins with structural domains called “zinc fingers“). Following iron, it is the most abundant trace element in the human body. The concentration of intracellular zinc is regulated by different cellular transporters.
Zinc deficiency, due to either hereditary or dietary causes, has been associated with skin alterations and delayed healing. Although dermatological disorders secondary to low levels of zinc in the body are normally resolved with oral supplements, this route of administration has not shown clear benefits in patients with wounds without this deficit. On the contrary, topical application of zinc has gained a good positioning between the alternatives of local treatment of wounds and perilesional skin.1,2
Let’s understand why.
What role does zinc play in wound healing?
The role of zinc in wound healing has been studied predominantly in experimental animal studies. In the skin, the highest concentration of zinc is found in the epidermis, especially in the keratinocytes closest to the basement membrane.
In the initial inflammatory phase, zinc levels rise at the edges of the wound and this concentration increases during granulation and epithelialization phase. This is due to increased expression of membrane transporters in keratinocytes, fibroblasts and macrophages. In the final stage of wound healing, these levels are reduced, with the consequent decrease in cell division..2
Although the exact action mechanism of zinc is unknown, different pathways in which it could be involved have been proposed, such as cell replication and migration (important role of zinc in the expression of the involved integrins), protein synthesis and cell repair. In addition, it has also been shown that topical zinc in wounds promotes autolytic debridement. This is due to the collagenase activity of the matrix metalloproteinases of which zinc is a cofactor. This benefit has been observed in pressure ulcers, diabetic foot and burns.1
On the other hand, zinc is also a cofactor of metalotioneins, antioxidant proteins that increase cellular resistance to apoptosis by having a protective effect against reactive oxygen species and bacterial toxins. Its anti-inflammatory effect is also associated with its regulatory action of macrophages and polymorphonuclear leukocytes.1
Although more studies are needed on its antimicrobial role, experimental studies have detected growth inhibiton of different bacterial species. However, resistance has been detected in certain strains, such as SAMR, and their ability to act on biofilms seems limited.1
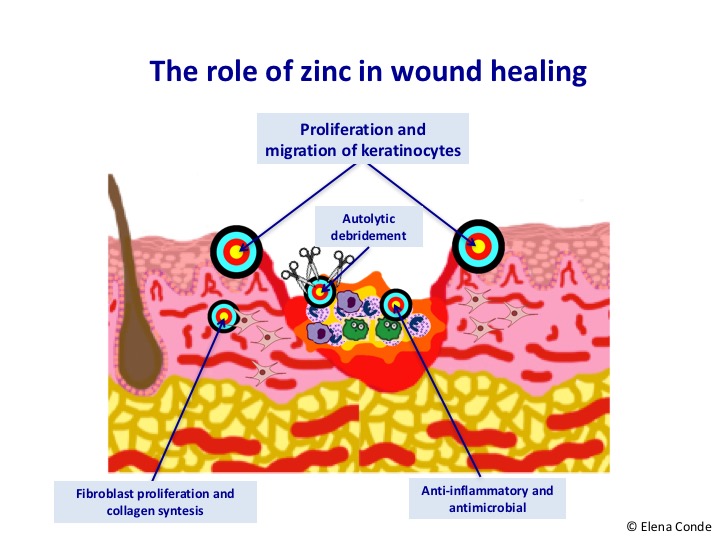
The conclusion would be that, when zinc is applied directly on the wound and damaged perilesional skin, the elimination of non-viable tissue is promoted, the risk of superinfection decreases, inflammation is reduced and epithelialization is stimulated. If we take into account that these effects are what we look for in all our patients, it seems like an interesting treatment, doesn’t it?
What is the interest of the topical application route?
Oral zinc sulphate supplementation is essential for healing in zinc-deficient patients. If normal levels exist, the conclusion of a systemic review of six clinical trials including leg wounds (with small sample size and different limitations) is that there is no benefit over placebo.3
On the contrary, its topical application has shown improvement at experimental and clinical level in patients presenting with both deficit and normal serum levels.
Zinc oxide or zinc sulphate?
Although zinc oxide and low zinc sulphate concentration have anti-inflammatory effects, experimental studies comparing these two presentations have demonstrated benefit of zinc oxide in wounds. The advantages over zinc sulphate, which is a water-soluble compound, are due to the fact that it enables a sustained release of zinc avoiding cytotoxic levels. Zinc oxide appears to simulate the action of certain growth factors, in addition to increasing its release.1
It is important to emphasize the astringent effect of zinc sulfate, which we frequently use in very exudative lesions. Zinc sulphate should always be used at low concentrations, as high levels of zinc sulphate inhibit epithelialization and increase inflammation.
How is topical zinc absorbed?
Percutaneous zinc absorption depends on the integrity of the epidermal barrier and the amount of zinc transporters in the cell membrane of the keratinocytes. Topical application of zinc, as well as topical corticosteroids, increase the concentration of these transporters and, therefore, the absorption of zinc.
Absorption depends on the zinc concentration of the preparation and the vehicle. Zinc oxide, when in contact with a humid and acidic environment, is hydrolyzed and releases zinc ions, which are those that have biological activity (Zn 2+). These ions progressively penetrate into the deep layers of the skin. Therefore, the application of zinc oxide products with a vehicle that promotes humidity and acidity, preferably in occlusion, optimizes the absorption of this ion. This explains the interest of bandages with zinc paste (boot of Unna). On eczematous skin, a constant situation in venous ulcer patients, zinc paste bandages form a protective barrier that decreases skin inflammation.1
What do clinical trials conclude?
Randomised controlled experimental studies that have been conducted to assess the interest of zinc in wounds are scarce. In pressure wounds, diabetic foot wounds and burns, as mentioned above, specific studies have been carried out, which have shown their debridement role.1,2
Considering leg wounds, a randomized clinical trial with 113 patients with venous ulcers compares 3 treatment arms: zinc paste bandage, zinc stockings and a calcium alginate dressing.4 In all cases a highly elastic bandage was also used. The authors associate the faster healing obtained in the zinc bandage arm with the benefit of compression due to the stiffness of the bandage. However, the potential benefit of topical zinc cannot be excluded.
Therefore, well- designed clinical trials are needed to analyse the real clinical utility of topical zinc in patients with leg ulcers.
References:
- Lansdown AB, Mirastschijski U, Stubbs N, Scanlon E, Agren MS. Zinc in wound healing: theoretical, experimental, and clinical aspects. Wound Repair Regen. 2007 Jan-Feb;15(1):2-16.
- Kogan S, Sood A, Garnick MS. Zinc and Wound Healing: A Review of Zinc Physiology and Clinical Applications. Wounds. 2017 Apr;29(4):102-106.
- Wilkinson EA. Oral zinc for arterial and venous leg ulcers. Cochrane Database Syst Rev. 2014 Sep 9;(9):CD001273. doi: 10.1002/14651858.
- Stacey MC, Jopp-Mckay AG, Rashid P, Hoskin SE, Thompson PJ. The influence of dressings on venous ulcer healing–a randomised trial. Eur J Vasc Endovasc Surg. 1997 Feb;13(2):174-9.
Also available in: Español (Spanish)