If I had to choose a single sentence to answer this question, it would undoubtedly be “with an adequate anti-inflammatory strategy and, if necessary, with an invasive approach”.
Some of you may have been surprised when Reading the term “invasive” associated with the word “gangrenous pyoderma”. In fact, the message we are used to is “pyoderma gangrenosum = no surgical debridement”.
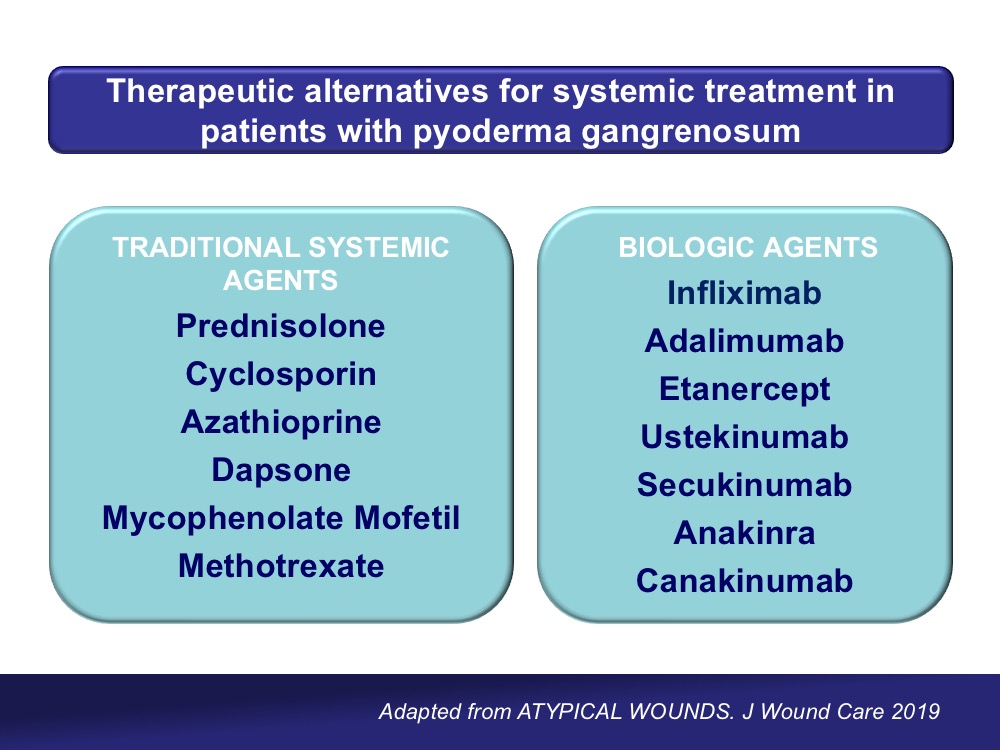
On the other hand, many of you will think that I am not saying anything new when talking about an anti-inflammatory strategy, because treatment with systemic and topical corticosteroids is the first choice in these patients (See post: Pyoderma gangrenosum: a diagnostic and therapeutic challenge).
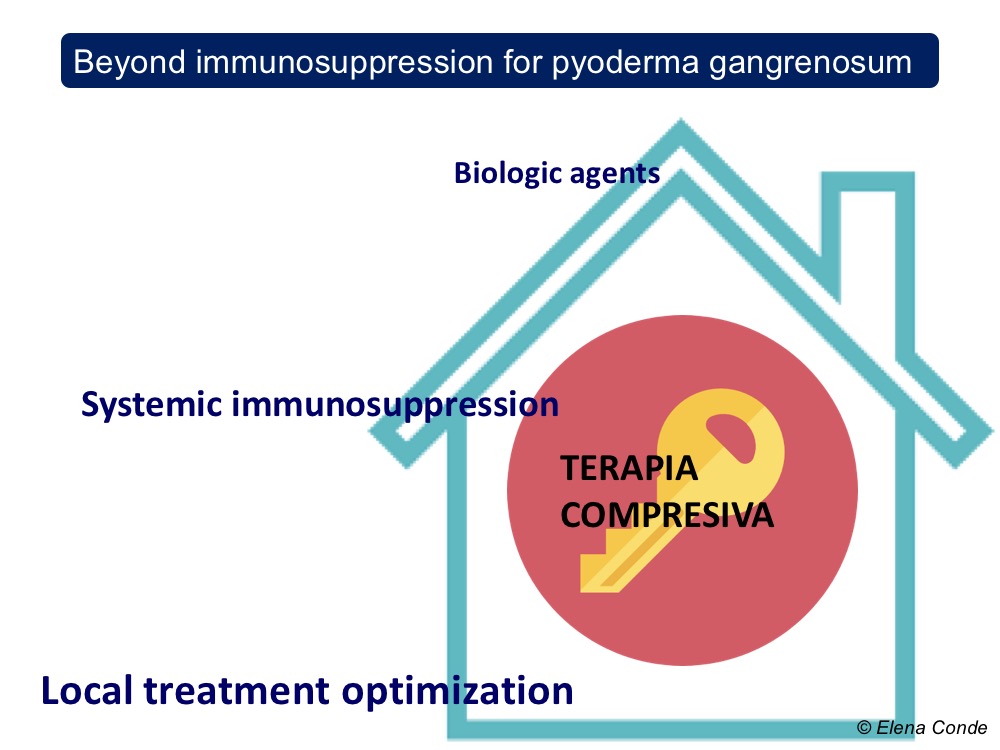
The aim of this post is to explain and underline the interest of a holistic approach to the patient with an ulcer secondary to pyoderma gangrenosum, beyond the use of immunosuppressive agents.
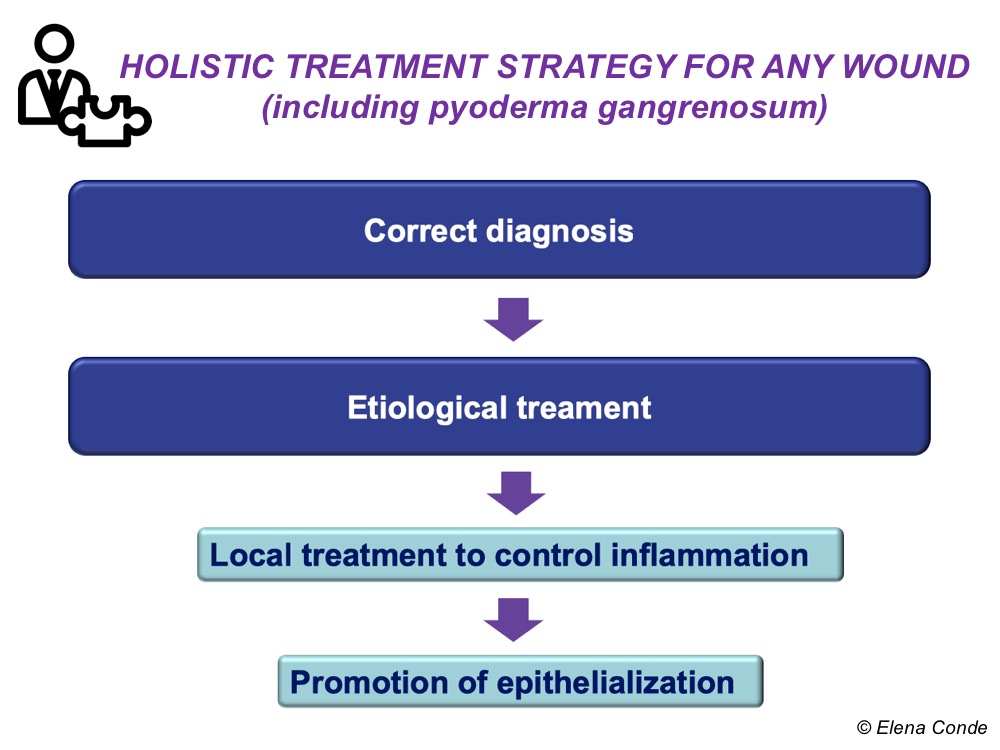
And we will explain it in 5 key points:
1. Compression Therapy
As we explained in the entry “Compression is key to treating leg wounds”, the inflammatory process inherent to any leg ulcer involves an alteration in microcirculation, with greater capillary filtration, and, due to the effect of gravity, an increase in intravenous pressure. Therefore, despite the absence of reflux or an obstructive disorder, the large inflammation found in pyoderma gangrenosum can trigger a state of venous hypertension that may hinder healing.
The interest of compression therapy in any leg injury is due to the following effects:
- Decreased capillary filtration
- Increased local lymphatic drainage
- Reduction of inflammation
- Increased arterial flow
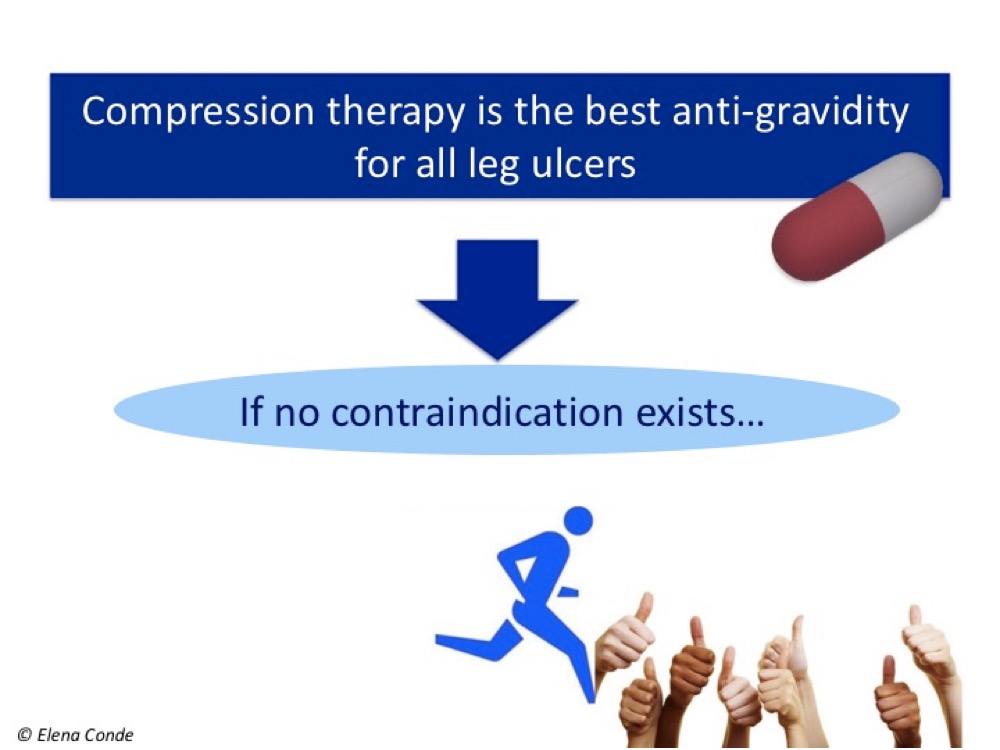
It is important to remember that the patient with an ulcer secondary to pyoderma gangrenosum (as with any other leg ulcer) may also have venous insufficiency or peripheral artery disease. In fact, in patients with pyoderma gangrenosum and chronic venous insufficiency, clinical worsening in spite of an adequate immunosuppressive treatment may be due to the pro-inflammatory effect of basal venous hypertension. As in the evaluation of any leg injury, pulse palpation is obligatory. In case of doubt, we will measure the ankle-brachial index (ABI).
So, which degree of compression would be necessary?
As underlined in the chapter on Pyoderma Gangrenosum in the EWMA’s document Atypical Wounds,1 there are no studies considering this topic. However, since the application of the compression bandage may be painful initially, the recommendation is to start with 20 mmHg and increase the compression depending on patient’s tolerance. With progressive reduction of inflammation, tolerance will increase. If the patient has concomitant artery disease, the type of compression will be adapted to it (see post “Compression is key to treating leg wounds”)
2. Promotion of a suitable wound bed microenvironment, wound edges and perilesional skin
As with any chronic ulcer, the choice of dressing type and frequency of dressing changes will depend on the characteristics of the wound bed and perilesional skin. Topical corticosteroids, like the systemic corticosteroids, is the etiological treatment of choice for pyoderma gangrenosum. Topical calcineurin inhibitors (tacrolimus) are an effective and safe alternative.
A holistic evaluation has to be carried out during each dressing change in order to detect and treat at an early stage the possible cause of clinical worsening. If there is more pain, extension of the lesion and perilesional erythema, in addition to thinking of a bad response to the treatment, the possibility of infection must always be assessed (the risk of infection is increased in these patients due to immunosuppressive treatment).
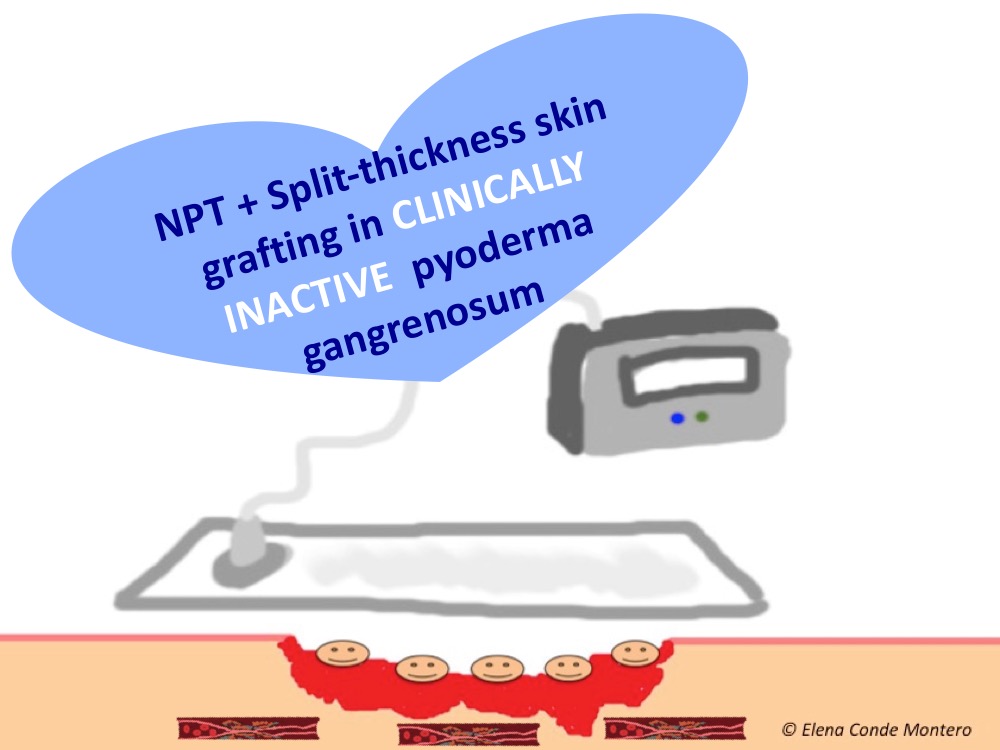
3. Negative pressure therapy and skin grafts
Complete healing rates with classical immunosuppressive treatments (predominantly oral corticosteroids and cyclosporine) do not reach 50% at 6 months. Although different biologic agents may be an effective alternative in non-responders, the problem is not only controlling pyoderma activity, but also repairing all lost tissue.
Once the inflammatory activity is controlled, the strategy to facilitate the formation of granulation tissue and promote epithelialization will be similar to that used in wounds of other aetiologies. Therefore, negative pressure therapy and thin split-thickness grafts will be good alternatives, either alone or in combination, to accelerate healing. This benefit is described in cases and small series published in the literature.2,3 In our clinical practice, as you can imagine, the type of skin graft that we normally use in these cases is punch grafting.
4. Topical Sevoflurane
Analgesic control is a key aspect in the treatment of wounds secondary to pyoderma ganrenosum, which are very painful lesions. Topical irrigation of sevoflurane is a very interesting option in these patients. Furthermore, as we commented in the post Have you ever heard of the topical use of sevoflurane in wounds?, this halogenated derivative of ether would not only have a beneficial analgesic effect, but it also has anti-inflammatory and healing properties (due to its vasodilator action).
La combinación secuencial de sevoflurano, terapia de presión negativa ambulatoria e injertos en sello es una constante en nuestra consulta.
5. Is it really a pyoderma gangrenosum?
Whenever an ulcer diagnosed as pyoderma gangrenosum does not respond to an adequate immunosuppressive treatment, besides considering that the ulcer may be resistant to treatment and could require association or change to other drugs, we should always wonder if “is it really an ulcer secondary to pyoderma gangrenosum?”
In fact, more than 10% of ulcers diagnosed as pyoderma gangrenosum are really other types of lesions4 … Among them, for example, vasculitis, Martorell ulcer, antiphospholipid syndrome and even factitious ulcers, which are also a diagnosis of exclusion (see post “Factitial ulcer: a silent cry for help“)

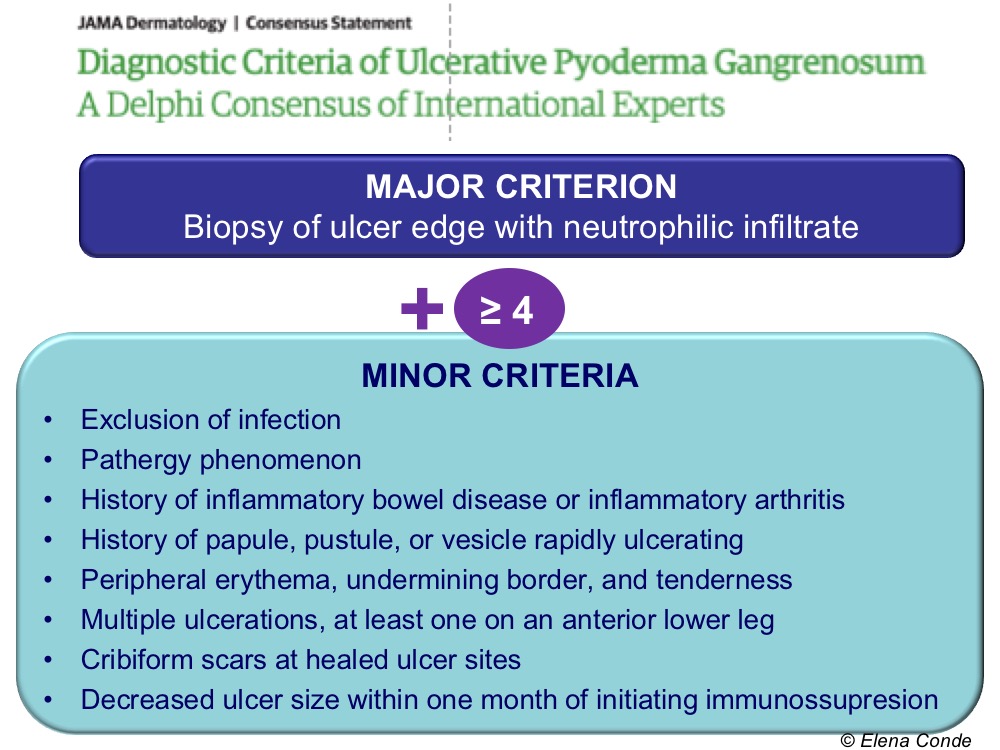
In order to stop considering pyoderma gangrenosum as a diagnosis of exclusion, different expert consensus on possible diagnostic criteria have been published. The most recent proposal includes, as we can see in the table, 1 major criterion (neutrophilic infiltrate in the biopsy) and the presence of 4 of the 8 minor criteria, with a sensitivity and specificity of 86% and 90%, respectively.5
I would like to end this post with my most sincere gratitude to the organizers and participants of the VI Congreso Nacional y V Internacional de Atención al Paciente con Heridas for the enormous affection, kindness and hospitality with which they have welcomed me in Medellin. IT HAS BEEN A FANTASTIC EXPERIENCE!
Referencias:
- Weenig RH, Davis MD, Dahl PR, Su WP. Skin ulcers misdiagnosed as pyoderma gangrenosum. N Engl J Med. 2002 Oct 31;347(18):1412-8.
- Maverakis E, Ma C, Shinkai K, Fiorentino D, Callen JP, Wollina U, et al. Diagnostic Criteria of Ulcerative Pyoderma Gangrenosum: A Delphi Consensus of International Experts. JAMA Dermatol.2018 Apr 1;154(4):461-466.
Also available in: Español (Spanish)














