Pyoderma gangrenosum is an inflammatory disease that leads to skin ulcers and its diagnosis and treatment can represent a real challenge for healthcare professionals.
Although it is not an infectious disease, the name pyoderma is maintained for historical reasons, since the hypothesis to explain the first cases described was that the lesions were secondary to an infection by organisms that produced pus (bacterial infection). The adjective gangrenous refers to the necrotic and destructive progression of the lesions.
And why is it a challenge? Essentially because we do not know many clues to understand the behaviour of this disease, it remains a diagnosis of exclusion and may be resistant to treatment.
As in order to diagnose a disease, clinical suspicion is the first step. Here we go!
Pyoderma gangrenosum typically occurs with the onset of single or multiple erythemato-violaceous pustules that rapidly progress to necrotic ulcers with an infiltrated purpuric rim. It can arise anywhere on the body. It may appear spontaneously or triggered by minor trauma or surgery.
Worsening of lesions following skin biopsy or surgical debridement of necrotic tissue is also typical. This hyper-reactivity is called pathergy phenomenon.
It’s a rare disease. It is more frequent in middle-aged patients, 30-50 years, with a slight female predominance. In addition to the classic form, ulcerative, pyoderma gangrenosum may have a bullous, pustular or vegetative presentation.
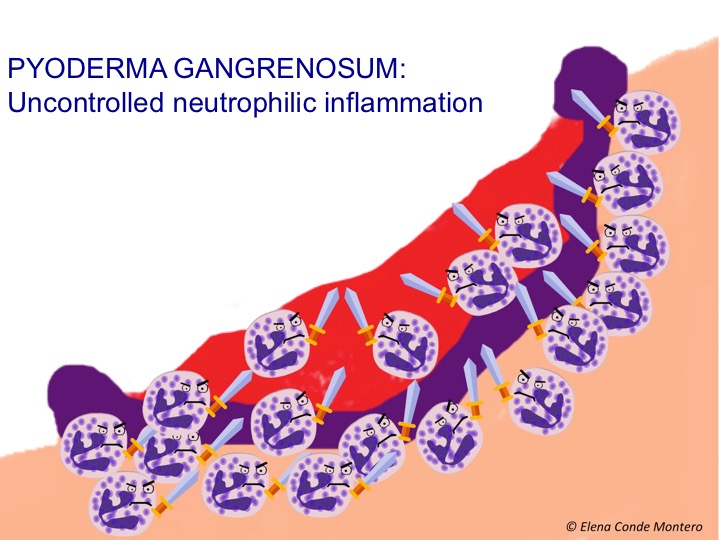
Pyoderma gangrenosum is an entity characterized by uncontrolled activity of the immune system cells, predominantly neutrophils, with production of necrosis and skin ulcers. Therefore, it is included in the group of neutrophilic dermatoses. In up to 50% of cases there may be associated systemic involvement, such as inflammatory bowel disease, arthritis or lymphoproliferative syndromes.
Regarding differential diagnosis, it is necessary to consider other diseases that may have a similar clinical presentation. Although pyoderma gangrenosum has typical histological findings (neutrophilic inflammatory infiltrate), they are not pathognomonic and may vary depending on the evolution of the lesion over time. It is therefore a diagnosis of exclusion. This implies that misdiagnosis may occur with other diseases (it is estimated that this occurs in 10% of cases).
Although wound progression may occur after biopsy, this procedure is needed to rule out other aetiologies that require management other than pyoderma gangrenosum.
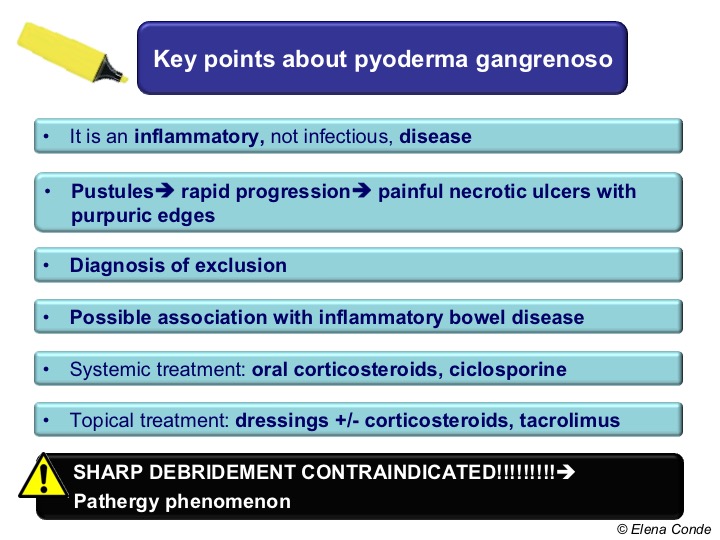
Pyoderma gangrenosum is treated with immunosuppressive drugs.
Prognosis is generally good, but recurrences are not uncommon.
Oral prednisone is considered the first line treatment. In cases requiring high doses of corticosteroids, or which do not respond satisfactorily, cyclosporine is recommended. In resistant lesions despite these immunosuppressive treatments, tumour necrosis factor alpha inhibitors (anti-TNF) may be an effective treatment alternative.
Now let´s go to the crucial point, how do we manage these wounds locally?
As in any wound, the use of dressings that promote healing in a moist environment is essential to facilitate autolytic debridement of necrotic and slough tissue, decrease pain, and enhance healing.
Treatment with local immunosuppressive drugs (corticoids or topical tacrolimus) will be indicated in superficial lesions or in patients with multiple comorbidities to avoid the risks of systemic immunosuppressive therapy. We already commented on this indication in the post “The role of topical corticosteroids in chronic skin wounds“.
Surgical debridement is contraindicated in these patients. However, when inflammatory activity has been controlled with adequate immunosuppressive therapy and the lesions are extensive, surgical debridement and skin graft coverage may be considered.
What is your experience with wounds secondary to pyoderma gangrenosum? Do you also consider it a diagnostic and therapeutic challenge?
Also available in: Español (Spanish)