When we find a necrotic plaque on a heel, the first thing that might come to our minds is “how do I remove it”… A SERIOUS MISTAKE! The first thing we must do is a holistic assessment of the person with the wound to diagnose the main cause and the factors that are influencing its evolution. If you were surprised by the title of this post, I hope that reading it will bring about a beneficial change in your clinical practice.
What is necrotic plaque in a heel and why can it occur?
Necrosis is defined as the pathological death of a group of cells or tissue by a harmful agent that has caused damage that cannot be repaired, i.e. it is irreversible. In the heel this occurs mainly due to ischaemia and/or pressure.
The necrotic plaque, also known as eschar, is formed by cellular debris, i.e. it is dead tissue that has lost its physical properties and its usual biological activity. It may have well-defined borders and be hard, dry and adherent to the wound bed or, on the contrary, be poorly demarcated and fluctuating on a sloughy and exudative wound bed. The drier it is, the more blackish the colour of this dead tissue, while the wetter it is, the more brownish it will become.
From the appearance of the necrotic plaque per se we cannot establish a diagnosis, as it is a non-specific type of lesion. Moreover, the presence of a necrotic plaque prevents us from knowing the true depth of the lesion (from superficial ulcers to bone involvement). It is therefore essential to take into account the clinical context of the patient (advanced age), their comorbidities (DM), their mobility and, most importantly, to explore the presence of peripheral occlusive arteriopathy. ANY HEEL WITH NECROSIS MUST BE PALPATED for DISTAL PULSES! Without a proper diagnosis of the main cause of the lesion and the factors that are influencing it, we will not be able to direct the treatment correctly.
Why should we not remove dry necrotic plaques from the heels?
Because when they are dry, adherent to the wound bed, without fluctuation or other signs of infection, they have a protective function. Keeping this protective plaque dry can prevent bacterial growth and have a “scab effect”. It also avoids the pain of sharp debridement and the possibility of exposing deep tissues (calcaneus) with potential for superinfection.
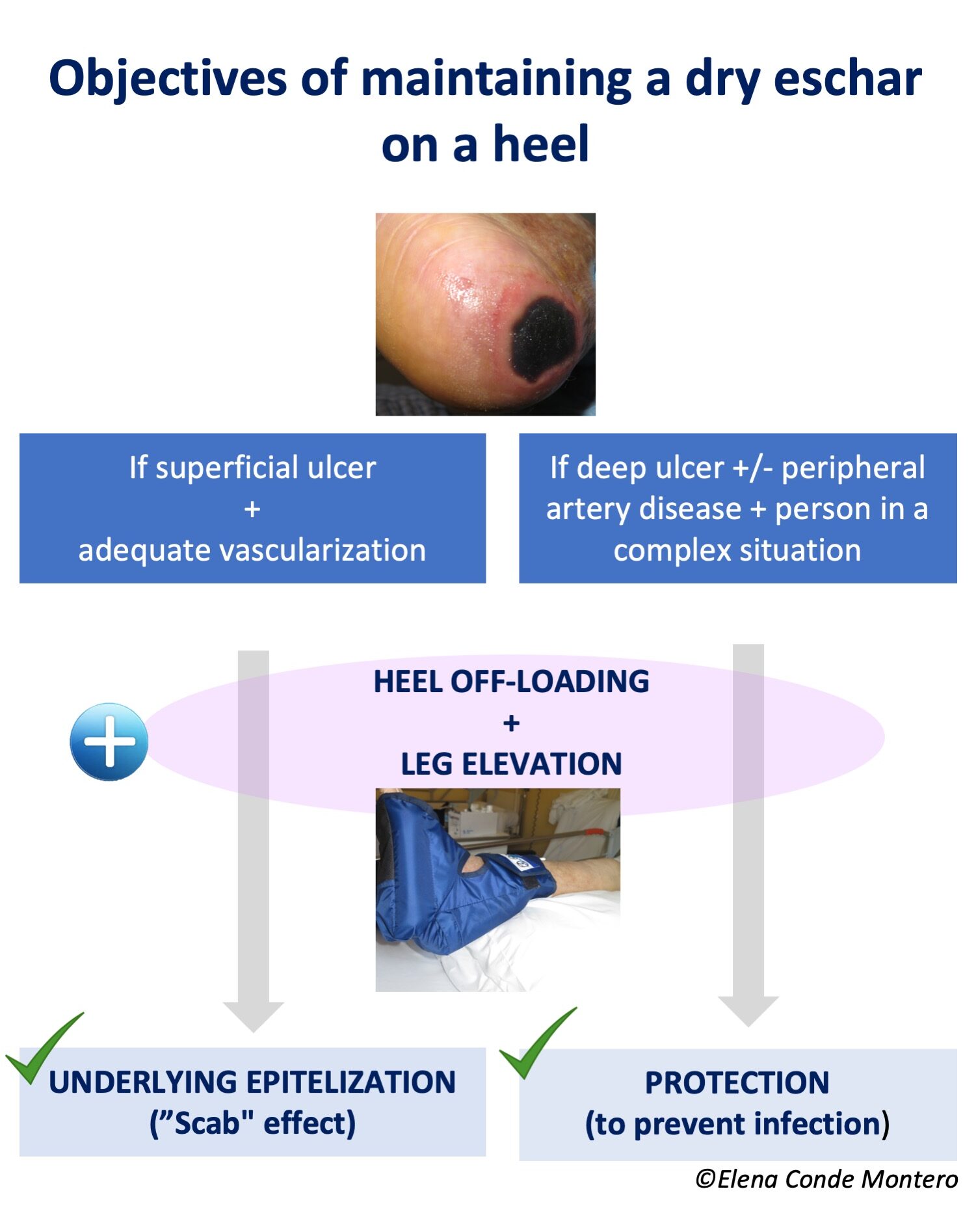
If the ulcer is superficial, not extensive and vascularisation is adequate, this scab could promote underlying epithelialisation. On the contrary, if the ulcer is deep and extensive, there is associated peripheral arterial disease and/or the complexity of the patient’s situation does not allow another approach that favours healing, the objective will be exclusively to maintain the “protective scab” to avoid superinfection (palliative protection or prior to revascularisation or amputation).
How do I keep these necrotic plaques dry?
With astringent and antiseptic products and avoiding anything that provides moisture.
If the scab is completely dry and adherent, the strategy is to leave it open air.
To promote drying, povidone iodine (see post: “Povidone iodine and chronic ulcers: a great controversy”) or calcium alginate fibre dressings for their “scab” effect (see post: “Why do we use so many alginate fibre sheets in our wound practice?”) are good alternatives.
DON’T FORGET THAT THE MOST IMPORTANT THING IS TO PREVENT CELL DEATH FROM PROGRESSING, SO PRESSURE RELIEF WITH HEEL PRESSURE RELIEF AND LEG ELEVATION WITH HEEL SUSPENSION ARE ESSENTIAL. IN ADDITION, IF THE MAIN CAUSE IS ARTERIOPATHY, THE VASCULAR SURGEON WILL ASSESS THE POSSIBILITY OF REVASCULARISATION.
Happy summer!
Also available in: Español (Spanish)






