Treatment of venous ulcers usually represents a great challenge, especially for dermatologists. At the “wounds session” of the EADV Congress in Paris, the dermatologist Sylvie Meaume, a prestigious wound specialist, presented a selection of articles published this year, the results of which are very interesting and could have an impact on our current therapeutic recommendations. I have selected 5 of them, in which the usefulness of the different strategies regarding etiological treatment and prevention of venous ulcer is evaluated.
1. Class 2 or class 3 compression stockings to prevent venous ulcer recurrence?

Several studies support the use of compression therapy to prevent venous ulcers recurrence, but it is remarkable the paucity of studies on the most effective type of compression.
This clinical trial aims to answer this question and compares an ankle pressure of 18-24 mm Hg (class 2) and 30-40 mmHg (class 3). Of the 361 recruited patients, 308 completed the study (170 men, 138 women; mean age 59 years). All had suffered venous ulcers, which had healed at the time for inclusion. Patients with arteriopathy, diabetes mellitus and ankle joint ankylosis were excluded. The study lasted 5 years, the first 2 with 24-hour use of the compression stocking, and the next 3 with exclusively daytime use. When comparing treatment adherence and recurrence rate at 5 years between the 2 groups, no significant differences were found in adherence, but recurrences were lower in patients with class 3 stockings (29% vs 60% in class 2 group), with longer disease-free time.
This study excludes the typical comorbidities of patients with venous ulcers, usually pluripathological elderly people, which are the ones that find it difficult to adhere to maintenance therapy with class 3 stockings. Therefore, as previous studies have shown that patients with adherence to compressive therapy, regardless of the class used, present fewer relapses, we must continue to recommend a degree of compression adapted to the needs of the patient. The class that we most recommend in our wound clinic is class 2, but for greater tolerance and compliance, in many cases we prefer class 1 stockings.
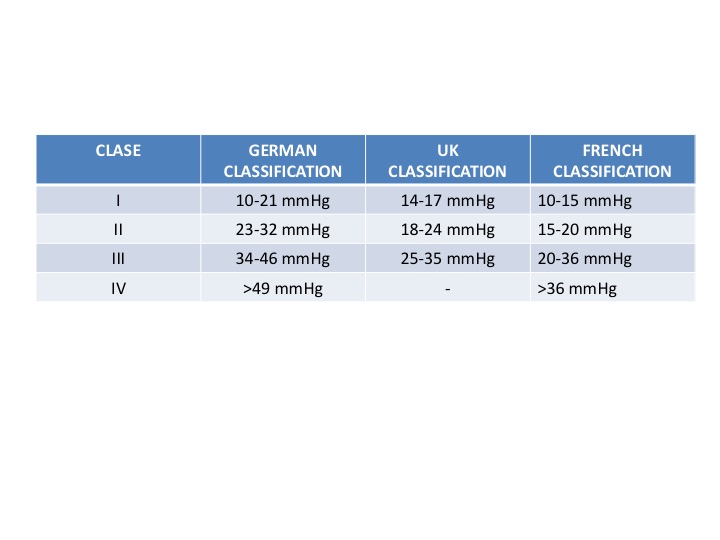
The following table is a small reminder of the pressure range to which each stocking class refers. Although the most used classification in Europe is the German one, taking into account the differences between countries, it is advisable to speak of mmHg and not of classes.
2. When to perform intravenous treatment, with open ulcers or after wound healing?
Venous reflux ablation is an essential weapon against venous hypertension. Surgery has shown a reduction in recurrences compared to isolated compression therapy (ESCHAR study. Lancet 2004). Endovenous treatments, such as sclerotherapy, are an interesting therapeutic alternative and its usefulness has just been evaluated in a clinical trial. The results of the Early Venous Reflux Ablation (EVRA) study indicate the benefit of early intravenous treatment for wound healing.
This 3-year multicentre randomized clinical trial included 450 patients divided into 2 groups: compression+ early endovenous treatment (within 2 weeks after inclusion) vs. delayed compression+ endovenous treatment (when the ulcer has healed or within 6 months of inclusion). The lesions were between 6 weeks and 6 months of evolution.
El tiempo medio hasta la cicatrización completa fue de 56 días en el grupo de tratamiento precoz vs 82 días en el tardía.
The mean time to complete healing was 56 days in the early treatment group vs 82 days in the late treatment group.
At 6 months, 85.6% and 76.3% of early and deferred treatment patients, respectively, had healed. Among patients with complete healing in the first year, the relapse rate was lower in the early reflux ablation group, with more disease-free days.
When analysing the good results of this study, it must be taken into account that the application of compression therapy (multicomponent, short-stretch bandages or compression stockings) was performed by specialized professionals, which may increase the effectiveness of the treatment.
The choice of the endovenous technique used (sclerotherapy or thermal ablation, alone or combined) depended on the criteria of each professional. So far no superiority of any endovenous ablation technique has been described, but in this study sclerotherapy was the most commonly used treatment.
Conclusion: the sooner the aetiology of the ulcer is treated, the better. However, in your clinical practice, is there a fast way to refer the patient to the specialist for early intravenous treatment?
3. Is the association between venous reflux ablation and compression therapy cost-effective?

Direct and indirect costs associated with leg ulcers have a high impact on the entire healthcare system, so assessing the cost of therapeutic interventions is essential. This paper is the first one to analyse the efficiency of adding reflux ablation to compression therapy. To this end, it analyses data from published clinical trials and obtains as a result that the combination of both treatments is the most efficient, with savings in total cost and benefit in quality of life. By preventing more recurrences, the cost of treatment would be amortized over the next 4 years or so. The biases of the different studies and the variability of venous disease in each patient must be taken into account (the response to ablation will be better in cases of isolated superficial reflux than in more complex cases).
Given that endovenous techniques (sclerotherapy, endothermic ablation) are currently spreading as an alternative to conventional surgery and studies point to their high efficiency, a comparative study of the costs associated with each procedure would be interesting.
A personal reflection: Despite the available evidence on its efficiency, how many of our patients are benefiting from this combined treatment?
4. Can I use compressive therapy in older patients with venous ulcers and arteriopathy?

This observational study includes 25 elderly patients (average age: 80 years), with different comorbidities (hypertension, diabetes mellitus) with venous ulcers (average duration of 18 months), peripheral arteriopathy and ITB>0.5, to study the tolerance of compressive therapy with short stretch bandages between 20 and 30 mmHg. No hemodynamic changes in measurements were found immediately after bandage placement and 24 hours later. No increased pain or skin signs of ischemia were detected. Therefore, as it had been suggested in previous studies, bandages with a high stiffness index with pressures less than 30 mmHg is a safe option in patients with peripheral artery disease and ITB>0.5. But watch out, always with a close follow up, listening to the symptomatology of the patient and inspecting the skin to detect early signs of ischemia!
5. Physical exercise is a common recommendation for our patients: is it evidence-based?

After the need for compressive therapy in venous ulcer patients, the recommendation we repeat most in our clinical practice is increased physical activity. How many studies have we read that support this recommendation?
This systematic review has just been published, which includes 6 clinical trials evaluating the benefit of exercise associated with compressive therapy. Most of them lasted 12 weeks. The studies include patients from different settings, variability in exercise programs and a small number of patients included (range of 13-184 patients). In addition, outcome variables vary between them. In none of the variables studied (time to healing, percentage of healed wounds, quality of life) significant differences were found between groups. No study measured pain, recurrences, associated costs, long-term outcomes or adherence to compressive treatment and exercise program.
Conclusion: We need more studies to detect which type of exercise regimen and how often it is most effective. In spite of these results, which arise from studies with different biases, a healthy lifestyle, with physical activity, must be a constant recommendation to our patients.
¿Cuál es tu lectura crítica de estos artículos?

Also available in: Español (Spanish)





