The annual congress of the European Academy of Dermatology and Venereology, has just been held in Madrid.This event is always a perfect occasion to meet European colleagues and friends.I really enjoyed organizing and participating in the wound management workshop ? Kirsi, Miriam and Cathelijn, we made a great team!
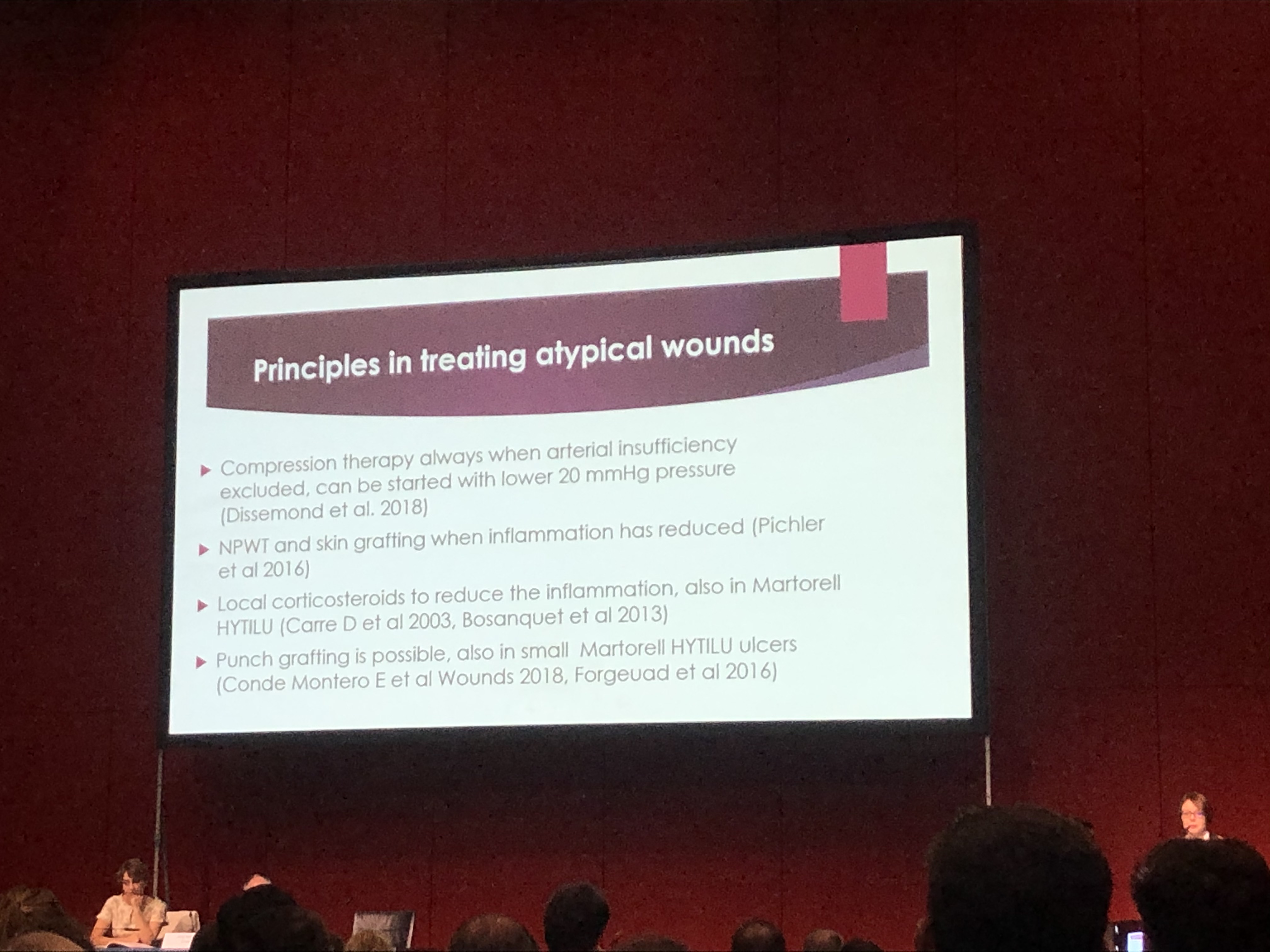
As expected, the session of the congress dedicated to ulcers had as protagonist the document recently published “Atypical wounds”. I encourage you again to read this work, as it can provide diagnostic and therapeutic pearls for those wounds of less frequent causes.
In addition to having a space for wounds, this European congress always has sessions dedicated to Phlebology. In fact, in different European countries, Phlebology is considered a subspecialty of Dermatology. I loved participating in one of these sessions talking about the causes of the different skin changes that can occur in the legs. Venous hypertension was, without a doubt, the “protagonist” cause of the skin alterations I presented. In the post “Chronic venous insufficiency from a dermatological perspective” I had already treated some of these changes, but, until now, I had not talked about two of them: white atrophy (“atrophie blanche”) and acroangiodermatitis. So let’s go!
Venous hypertension was, without a doubt, the “protagonist” cause of the skin alterations I presented. In the post “Chronic venous insufficiency from a dermatological perspective” I had already treated some of these changes, but, until now, I had not talked about two of them: white atrophy (“atrophie blanche”) and acroangiodermatitis. So let’s go!
White atrophy (atrophie blanche) secondary to chronic venous insufficiency
What is white atrophy?
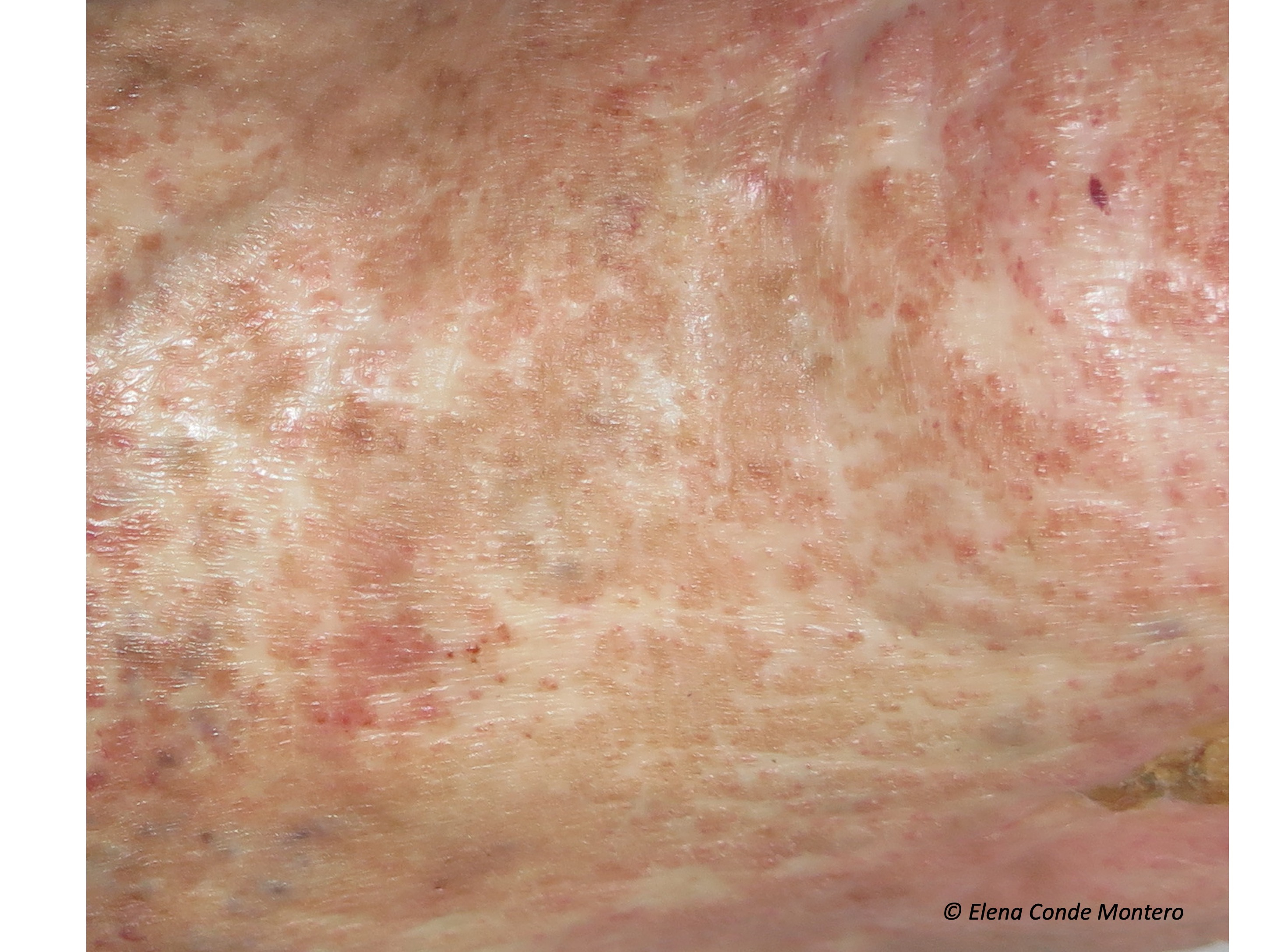
White atrophy (or “atrophie blanche”, which is the French term with widespread use) is the way to call atrophic stellate, porcelain white plaques, with red dots inside (dilated vessels), which can appear on the leg and foot for different reasons. That is to say, it is a term that must be used to describe a cutaneous alteration of cicatricial aspect, which is not pathognomonic of any disease, since it can appear in several clinical situations. Therefore, it is essential to make a detailed clinical history whenever we find it. White atrophy is usually painful and, if ulcers develop in that area, their healing tendency will be limited.

Why does it occur?
It is not known exactly, but it is usually associated with the alteration of the microcirculation. The authors who have histologically studied these lesions initially describe occlusions of the small vessels of superficial dermis with fibrinous microthrombi, hyalinization and wall thickening and, in lesions of longer evolution, dermal sclerosis and epidermal atrophy.
Therefore, all those diseases that produce this type of decrease in microcirculatory flow can trigger “tissue infarcts” and the consequent “scar areas”, which we call white atrophy. Chronic venous insufficiency is one of these diseases and, in fact, the one most associated with white atrophy.
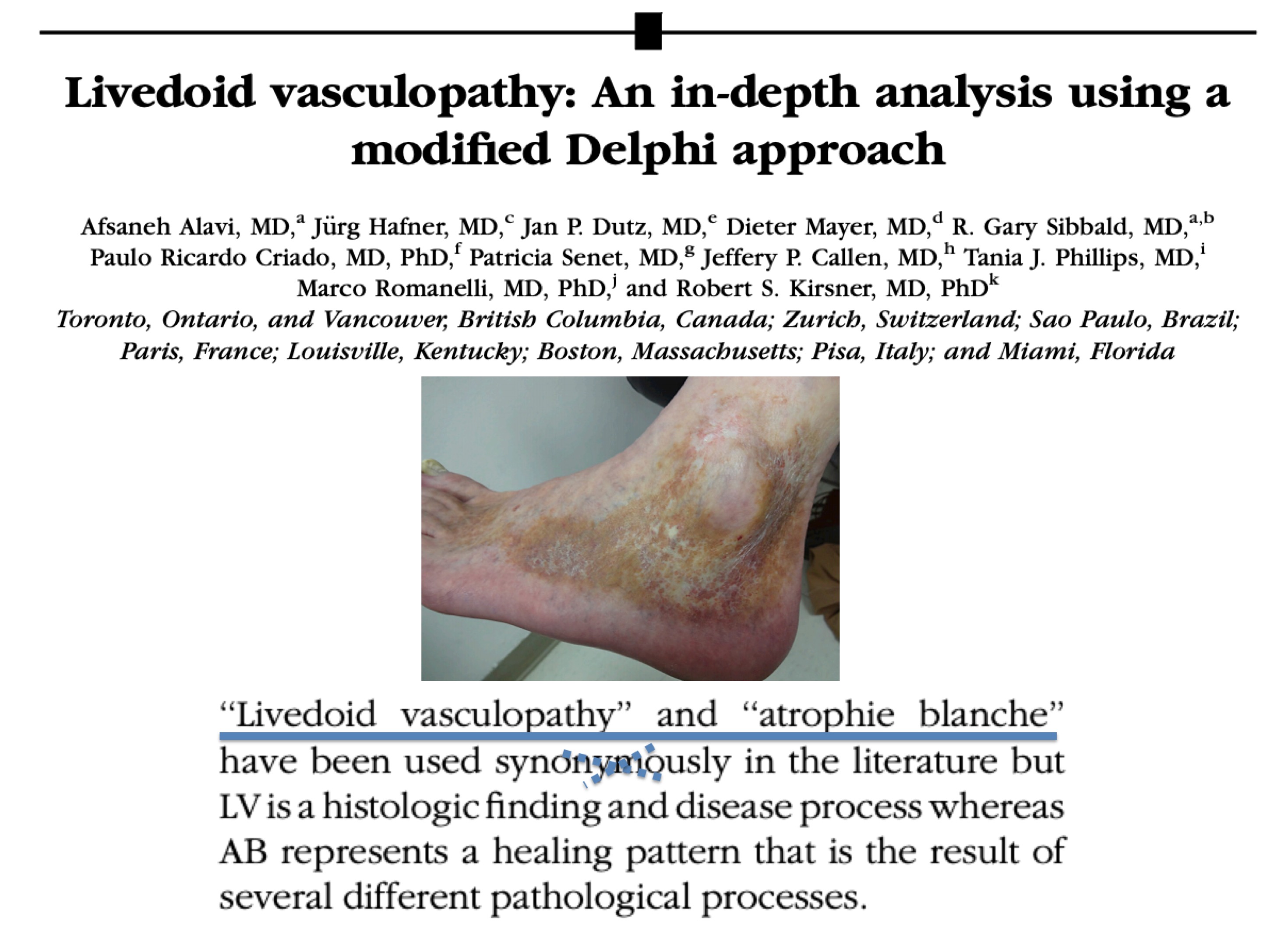
However, it may appear secondarily to other disorders involving coagulation disorders (hypercoagulability states, collagen disorders, alteration of fibrinolysis) and even in a primary presentation. All of these primary and secondary causes of white atrophy would be included within the entity known as livedoid vasculopathy, a type of occlusive vasculopathy without associated vasculitis. In many patients with white atrophy and a diagnosis of livedoid vasculopathy, we also find chronic venous insufficiency. Livedoid vasculopathy usually affects middle-aged women and presents with painful purpuric papules, typically on the dorsum of the feet and inframaleolar region, progressing to ulcers and areas of white atrophy. Therefore, in cases of white atrophy without associated chronic venous insufficiency, we should perform both lab tests to exclude thrombophilia and biopsy of the edge of the ulcerated lesions.
So, why is the term white atrophy used as a synonym for livedoid vasculopathy?
Because the lesions of white atrophy are very striking in this type of occlusive vasculopathy. However, as we have seen, white atrophy is not exclusive to this disease and, in addition, livedoid pathology is an entity with many points of controversy. Conclusion, they should not be used as synonyms.
How should white atrophy be treated?
The treatment will be that of the associated disease and the objective will be, mainly, to avoid the progression of the lesions. In cases of chronic venous insufficiency, the control of venous hypertension is essential, with anti-edema measures, compressive therapy and, if possible, intravenous treatment (sclerotherapy or thermal ablation techniques). Compressive therapy must be adapted to the patient’s tolerance, as these lesions can be very painful.
Acroangiodermatitis secondary to chronic venous insufficiency
Although acroangiodermatitis (called acroangiodermatitis of Mali, the surname of the person who described it) is usually considered infrequent, this error in the estimation of its prevalence may be due to an underdiagnosed disorder. The truth is that in our wound consultation we see it frequently.
What is acroangiodermatitis?
It is a reactive proliferation of small vessels in response to a chronic vascular alteration, such as poorly controlled venous hypertension. Therefore, its most frequent location is the foot and leg. As it can also appear secondarily to arteriovenous malformations or fistulas, it can develop in upper extremities.
How does it occur?
Initially, eritemato-purpuric or brownish macules usually appear, which evolve to the formation of papules or plaques that can become warty and ulcerated. The discomfort is very variable, from asymptomatic to very painful lesions. They usually involve the back of the foot, affecting the toes and ankle, including the malleolar area. However, it can also appear on the leg. It can be uni or bilateral, depending on the evolving stage of chronic venous insufficiency in each limb.


Its clinical presentation may be similar to other diseases that should be included in differential diagnosis, especially hyperpigmentation by haemosiderin deposits or Kaposi’s sarcoma.
How is acroangiodermatitis diagnosed?
The confirmation diagnosis will be obtained by performing a skin biopsy of the lesions. Histologically, acroangiodermatitis is characterized by a proliferation of endothelial cells and an increase in the number of pericytes (perivascular spindle cells) in the dermis. The use of two immunohistochemical stains will help us to differentiate it from Kaposi’s sarcoma. CD 34 staining is only positive in endothelial cells in acroangiodermatitis, whereas in Kaposi sarcoma it also stains perivascular cells. In addition, Human Herpesvirus-8 staining is negative in acroangiodermatitis.
How is it treated?
Treatment of acroangiodermatitis secondary to chronic venous insufficiency is the control of venous hypertension. Therefore, we will insist on anti-oedema measures and the use of adequate therapeutic compression. As in the case of white atrophy, the objective will be to slow down the evolution of the disease.
References:
- Alavi A, Hafner J, Dutz JP, Mayer D, Sibbald RG, Criado PR, Senet P, CallenJP, Phillips TJ, Romanelli M, Kirsner RS. Atrophie blanche: is it associated with venous disease or livedoid vasculopathy? Adv Skin Wound Care. 2014 Nov;27(11):518-24; quiz 525-6.
- McVittie E, Holloway S. Aetiology and management of atrophie blanche in chronic venous insufficiency. Br J Community Nurs. 2015 Dec;20 Suppl 12:S8-S13.
- van Montfrans C, De Maeseneer MGR. Atrophie Blanche (C4b) Can Be Reversible After Targeted Treatment. Eur J Vasc Endovasc Surg. 2019 Sep;58(3):435.
- Badahdah HM, Edrees KM, Alnasr L, Junainah E. Acroangiodermatitis of Mali(Pseudo-Kaposi Sarcoma) Associated with Chronic Venous Insufficiency and Obesity: A Case Report. Wounds. 2018 Nov;30(11):E105-E107.
Also available in: Español (Spanish)











