Homocysteine is an amino acid that is not present in dietary proteins, but is formed exclusively as an intermediate product in the metabolism of methionine to cysteine and participates in the folate cycle and DNA methylation. If there is any mutation in the enzymes involved or there is an acquired deficit of essential vitamins in these metabolic processes, homocysteine blood levels increase.
High blood levels of homocysteine (hyperhomocysteinemia) are considered a risk factor for arterial and venous thrombosis.
Vascular alterations produced by homocysteine are thought to be multifactorial. Homocysteine causes direct damage to the endothelium, stimulates lipid peroxidation and increases platelet aggregation. In addition, this amino acid promotes inflammation in vessels by releasing pro-inflammatory cytokines and stimulating leukocyte adhesion to endothelial cells, with consequent migration to surrounding tissue.1
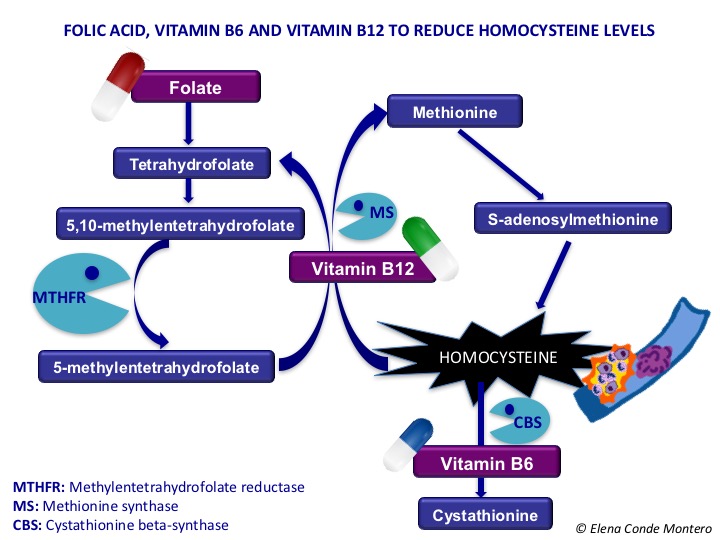
As we can observe in the following scheme, the activity of the enzyme methylenetrahydropholate reductase (MTHFR), involved in the folate cycle, is essential for the reconversion of homocysteine into methionine. The polymorphisms of this enzyme can decrease its action and, therefore, increase the concentration of homocysteine in the blood. The C677T mutation (mutation in a single nucleotide) is the most frequent polymorphism and is an independent risk factor for thrombosis, even with normal homocysteine levels in the blood. In patients with coronary artery disease or hypertension its prevalence increases to 25-35%. Risk increases when cellular folate levels decrease.2 Thrombophilia and vasculopathy associated with hyperhomocysteinemia may be the trigger for skin wounds.3
Higher serum homocysteine levels have been detected in patients with chronic venous insufficiency (with or without ulcer) than in patients without this underlying disease. Therefore, elevation of serum homocysteine may be implicated in the pathogenesis of stasis dermatitis and its progression to ulceration.1 Another study has shown the benefit in healing of daily folic acid supplementation in cases of venous ulcer and hypermicysteinemia.4
Regardless of their possible role in chronic venous insufficiency, cases of pyoderma gangrenosum-like necrotizing lesions caused by disorders in homocysteine metabolism have also been reported.2
Diagnosis of pyoderma gangrenosum is a diagnosis of exclusion. Clinically it can be confused with different diseases. Normally we have in mind the most frequent differential diagnoses: vasculitis, occlusive vasculopathy, infections, malignancies, Martorell ulcer, even factitious dermatitis. It is important that the skin biopsy is sufficiently broad and deep to exclude these diagnoses, as many share the typically neutrophilic inflammation that can be seen histologically in pyoderma gangrenosum.
However, the diagnostic key is not always provided by biopsy, as in the case of alterations in homocysteine metabolism. It is important to know this pathology in order to suspect it in patients with these diagnoses who do not respond as expected to treatment.


Right lateral leg ulcer and necrotic scabs with erythemato-violaceous halo on the left lateral leg in the context of hyperhomocysteine (lesions previously diagnosed as pyoderma gangrenosum without response to immunosuppressive treatment).
We need to request homocysteine blood levels. However, it is important to know that, despite normal homocysteine levels, a patient may have a mutation in the MTHFR enzyme and therefore an alteration in the metabolism of this amino acid with clinical repercussions. 2 In this case, with clinical suspicion, despite normal homocysteine levels, mutation in the MTHFR gene must be requested. Treatment with vitamin B6, vitamin B12 and folic acid supplementation may reduce homocysteine levels, even in patients with normal serum concentration of these vitamins.2,3
Undoubtedly, considering the simplicity and good tolerance of treatment, it is very interesting to go deepler into the potential role of alterations in homocysteine metabolism in recalcitrant ulcers in patients with risk factors and history of cardiovascular events.
Have you diagnosed any cases of ulcers in the context of hyperhomocysteinemia / MTHFR mutation?
Referencias
Also available in: Español (Spanish)






