A burn is a very common type of traumatic wound, whose healing process can be pathological, with the appearance of a hypertrophic or keloid scar. Intralesional corticosteroid infiltration is a technique of choice for treating pathological scars. Therefore, considering the known risk of hypertrophic scarring after a burn, could it be interesting to apply topical corticoid in a preventive manner? The authors of an article published in 20141 ask this same question and conclude that ” Theoretically, topical corticosteroids could reduce pathological scarring by decreasing inflammation and activation of fibroblasts. However, there are no studies evaluating this hypothesis”.
Despite the absence of studies on this subject, we will understand the reason of this interesting reflection. To this end, we begin with a brief introduction to burns.
How are burns classified?
Depending on the depth of skin involvement, burns are classified in different degrees:
- First degree: only the epidermis is affected. Usually only erythema occurs and heals without leaving a scar.
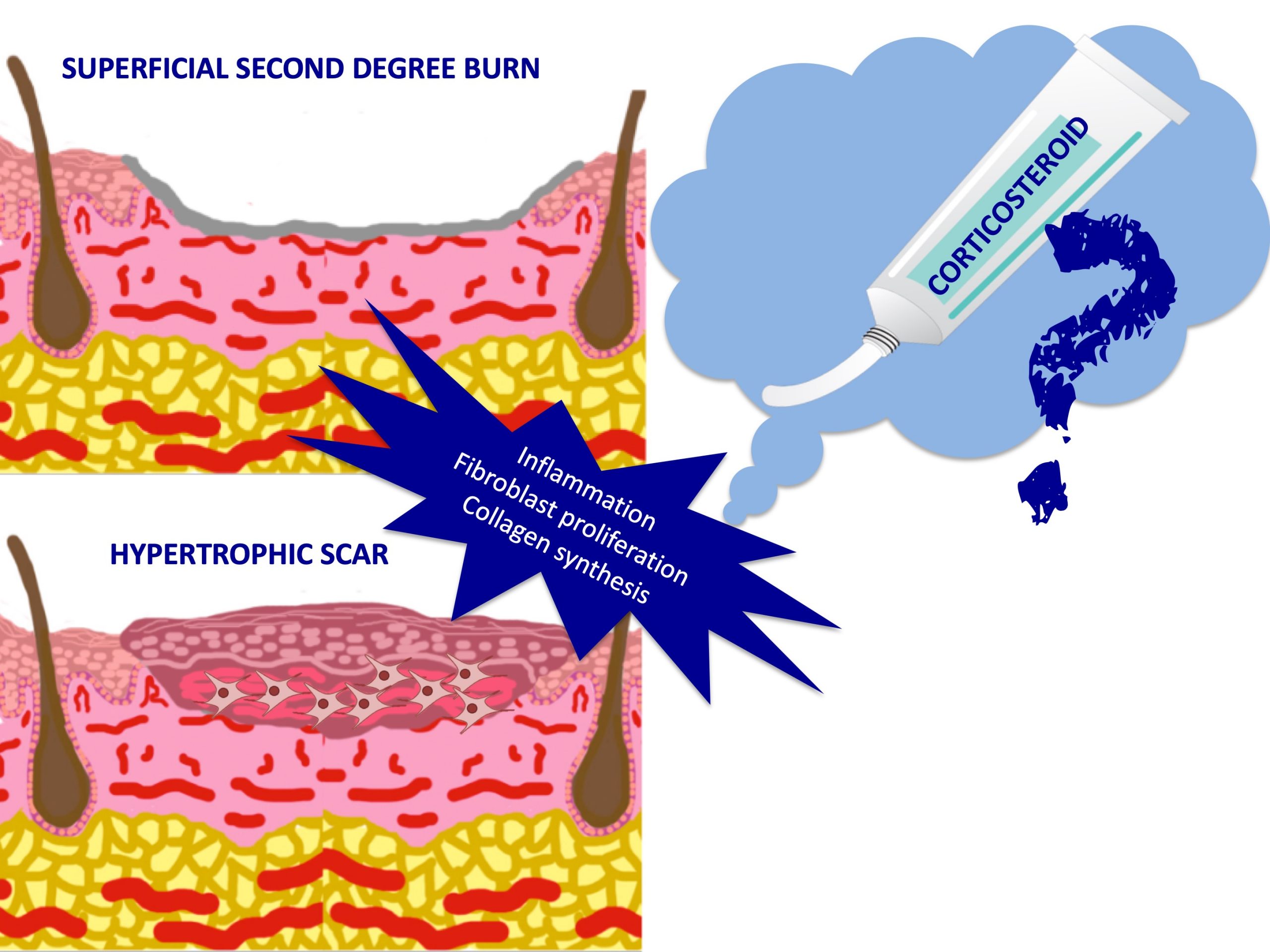
- Second degree: affects epidermis and dermis with the formation of a blister. Depending on the depth of the affection of the dermis, they are divided into superficial and deep, normally the bottom of the blister being red in the former and whitish in the latter. The risk of developing a hypertrophic or keloid scar is greater the deeper the involvement.
- Third degree: it implies a necrosis of all the skin layers. Graft coverage must be performed to avoid contracture and hypertrophy.
In addition to the depth of the affectation, to measure its severity, its extension, location, type of burn, age and associated pathologies of the patient must be taken into account.
We will now focus on a type of burn that we frequently encounter in our daily lives, superficial second-degree burns.
What is the healing process after a burn?
As in any wound, after the damage produced by a burn, a process begins in which the cells and molecules involved vary over time. Therefore, to facilitate its study, the healing process is divided into phases, although these phases actually overlap (see post “Brief overview of wound healing”)
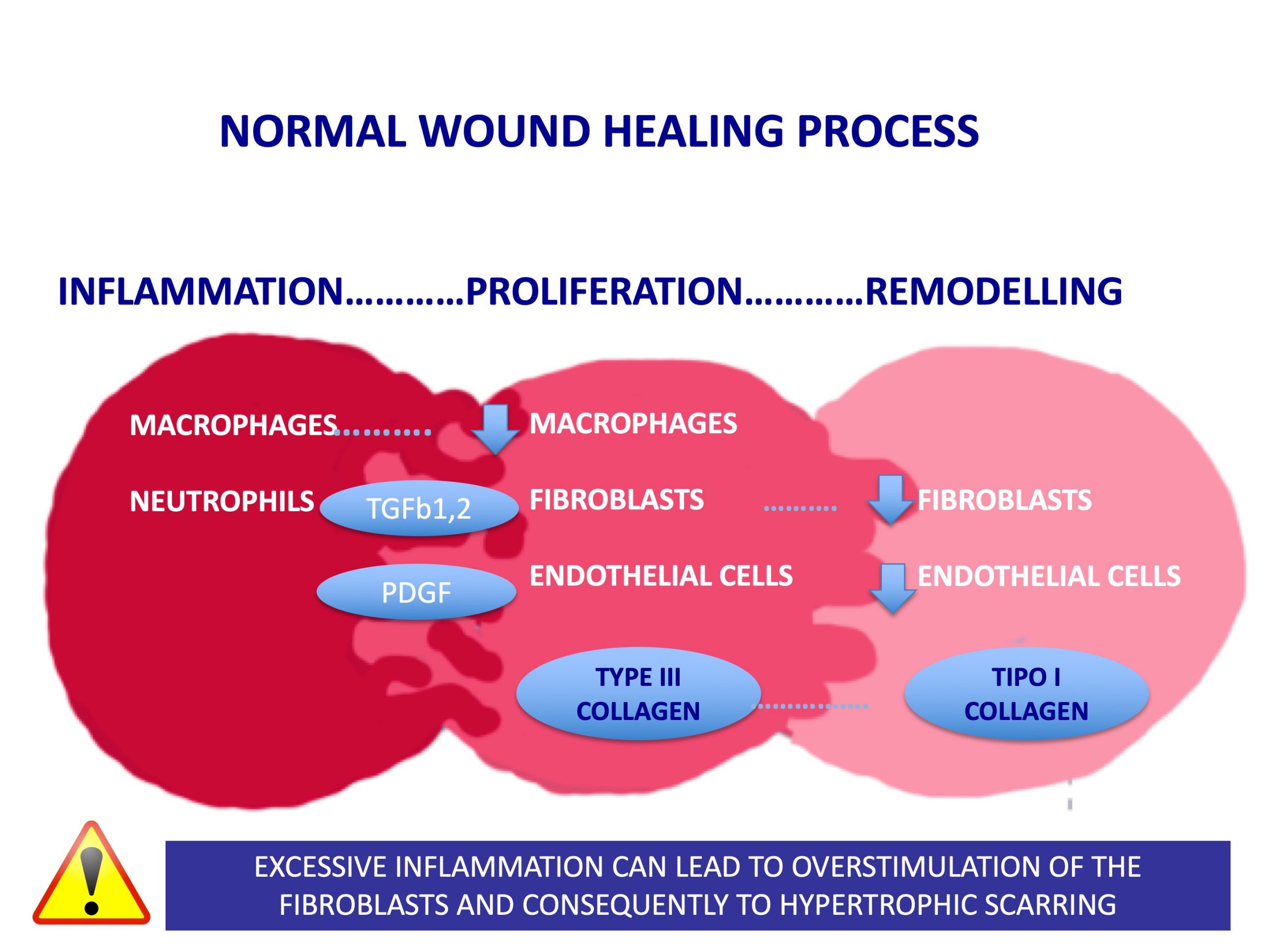
In the inflammatory phase, macrophages are first responsible for creating a pro-inflammatory environment, releasing cytokines such as IL-1 and TNF, and they engage in phagocytosing bacteria and destroying devitalised tissue. Later, in the proliferative phase, macrophages differentiate to secrete growth factors (TGFb1 and 2, PDGF) that stimulate the proliferation of fibroblasts and their production of collagen (type III collagen), as well as the proliferation of endothelial cells for the formation of new vessels. In the final or remodeling phase, apoptosis of the cells formed for the proliferation of new wound tissue occurs and type III collagen is degraded to form type I collagen. This collagen is organized differently than normal skin collagen, but over time the appearance and function of the scar can be improved.
If excessive scar tissue has been produced, a hypertrophic scar (red, raised, that worsens months after wound production and improves spontaneously over the next 1-2 years) or a keloid (extends beyond the limits of the original wound and does not improve without treatment) may develop.
With respect to other types of wounds, burns are injuries with a high risk of pathological healing, mainly if there is deep dermis involvement. This higher incidence of hypertrophic or keloid scars in burns seems to be associated with the intense and prolonged inflammation that usually occurs in this type of wounds and the consequent excessive proliferation of fibroblasts and collagen production.
Why and how should topical corticosteroids be applied to prevent pathological scarring?
Topical corticosteroids decrease the synthesis and release of inflammatory mediators (including prostaglandins and cytokines such as IL-1 and TNF), reduce the release of growth factors that stimulate fibroblast proliferation (TGFb1, TGFb2, PDGF) and thus decrease collagen production. Thus explained, it seems an interesting preventive strategy to prevent a pathological scar in a superficial burn. However, when to start? and how long to maintain it? These are difficult questions to answer, essentially because scar hypertrophy can occur months after the burn. In fact, the authors of the article with which I started this post,1 propose the use of topical corticosteroids after epithelialization to limit possible persistent inflammation in the dermis, which would be responsible for excess fibroblasts and collagen causing hypertrophy.
The few studies that have been published on topical corticosteroids in first and second degree superficial burns do not help us to answer these questions, as they focus on its analgesic and early anti-inflammatory effect. Some authors propose the benefit of its early and time-limited application (a few days) to decrease inflammation and pain without affecting subsequent epithelialization. However, two clinical trials with healthy volunteers (15 and 20 volunteers included) found no improvement with respect to placebo when applying medium or high potency corticosteroids in the first 24 hours2 or daily for the first 3 days after the burn3.
And what do the guidelines say about topical corticosteroids in superficial burns?
The guidelines produced by the Japanese Dermatology Association,4 published in 2016, make recommendations on the use of topical corticosteroids in first- and second-degree superficial burns. It is stressed that its use in this indication is based on its anti-inflammatory activity and that, despite the lack of available evidence, it is a widely used treatment in clinical practice and recommended by experts.
What is your experience? Do you recommend medium or high potency topical corticosteroid cream for superficial second-degree burns? Early or after epithelialization?
Referencias:
Also available in: Español (Spanish)






