Atypical wounds are in vogue this year… No doubt the document “Atypical Wounds”, led by Kirsi Isoherranen and supported by the EWMA, has a lot to do with this “trend” ?. As I said in previous posts, I loved being part of this publication, which I consider fundamental (and written in a simple and attractive way) for all of us who treat patients with wounds. The dissemination of the document is also being a fantastic experience and a perfect excuse to exchange impressions between experts from different European countries (this week in Geneva and Galway). The multi-perspectivism is enormously enriching both professionally and personally.
I was delighted to participate in the seminar on injuries organised in Galway by the Alliance for Research and Innovation in Wounds. A great format, with the participation of health professionals, patients and engineers to solve fundamental questions: What do the GUIDELINES say? What happens in PRACTICE? What solutions does TECHNOLOGY give us? And, most importantly, what do PATIENTS feel and think? Congratulations, Georgina Gethin and team, for the perfect organization of the seminar!

I have decided to dedicate this entry to atypical wounds with necrotic tissue, in the wound bed and/or on the edges, as this is the type of clinical presentation that “scares” us the most in the clinical practice. Necrotic tissue is made up of dead cells and denatured proteins, it can be more or less humid and its coloration varies from black to brownish. When we find it, we have to find out the cause of cell destruction. The purplish border is an indicator that tissue perfusion is altered by an occlusive and/or inflammatory process. Inflammation may be inside and/or outside the vessels.
Many things may be happening, but before thinking about less frequent causes, the first thing to do is to palpate foot pulses and rule out the possibility of an ulcer with an arterial component.
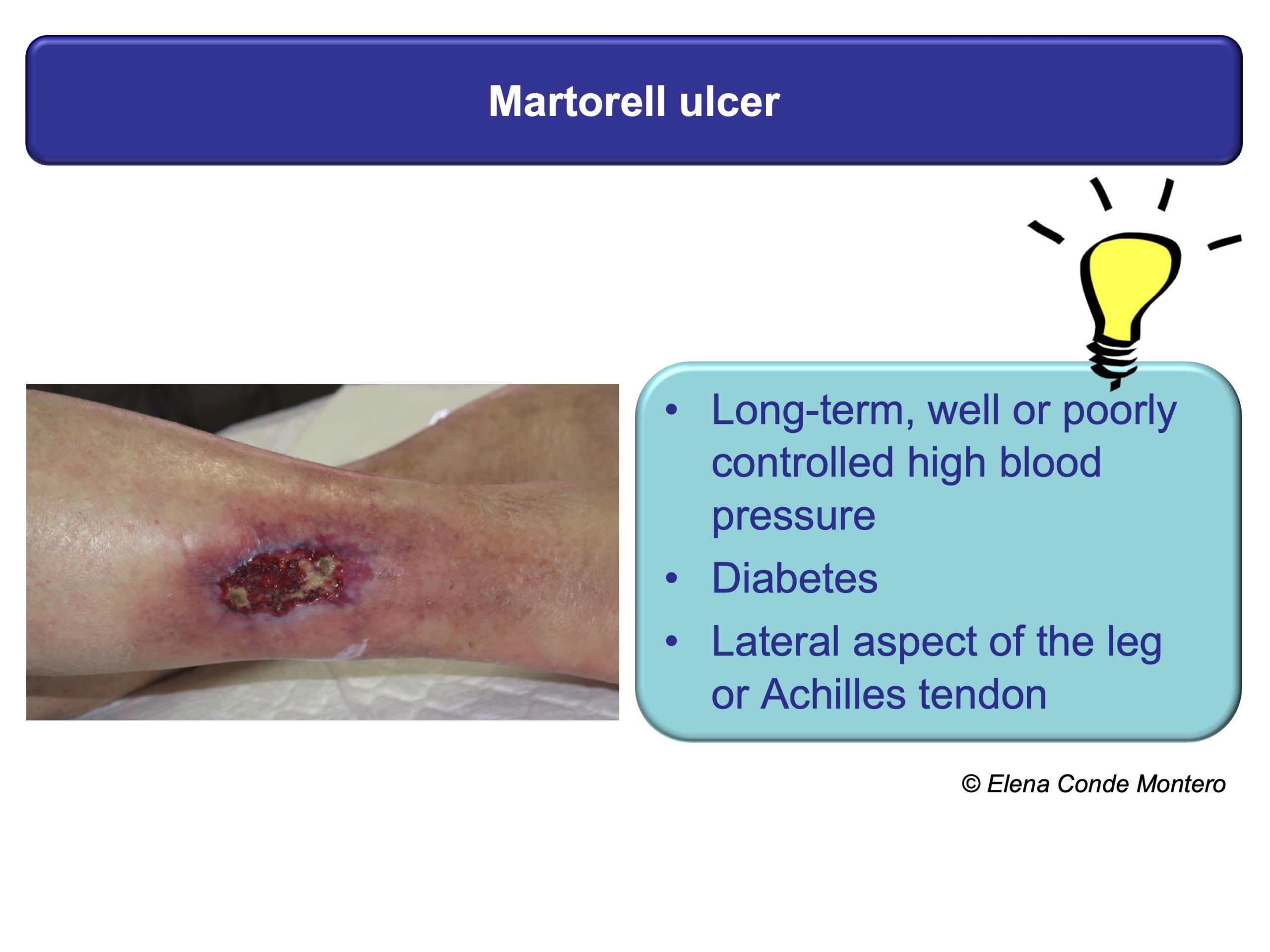
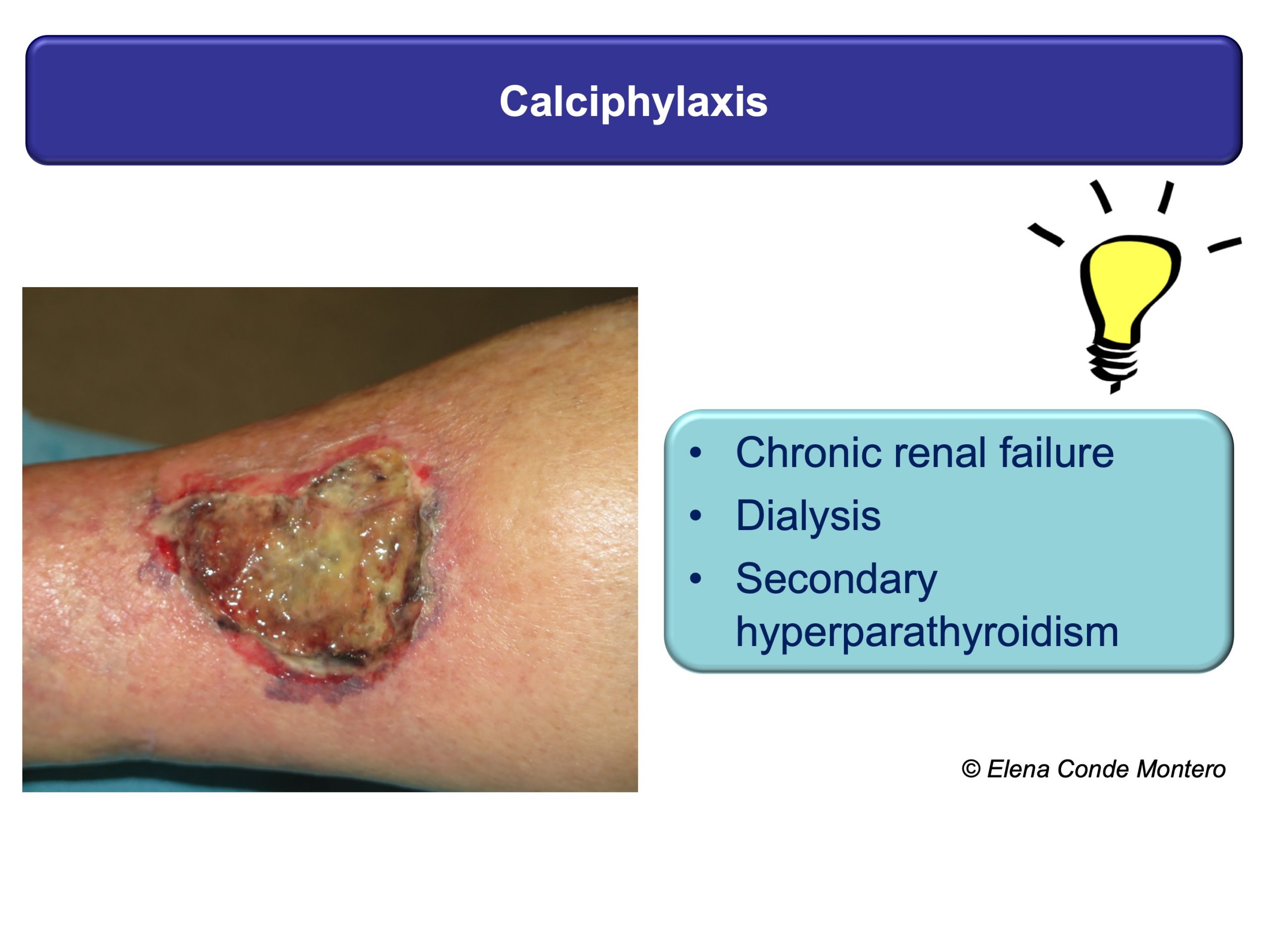
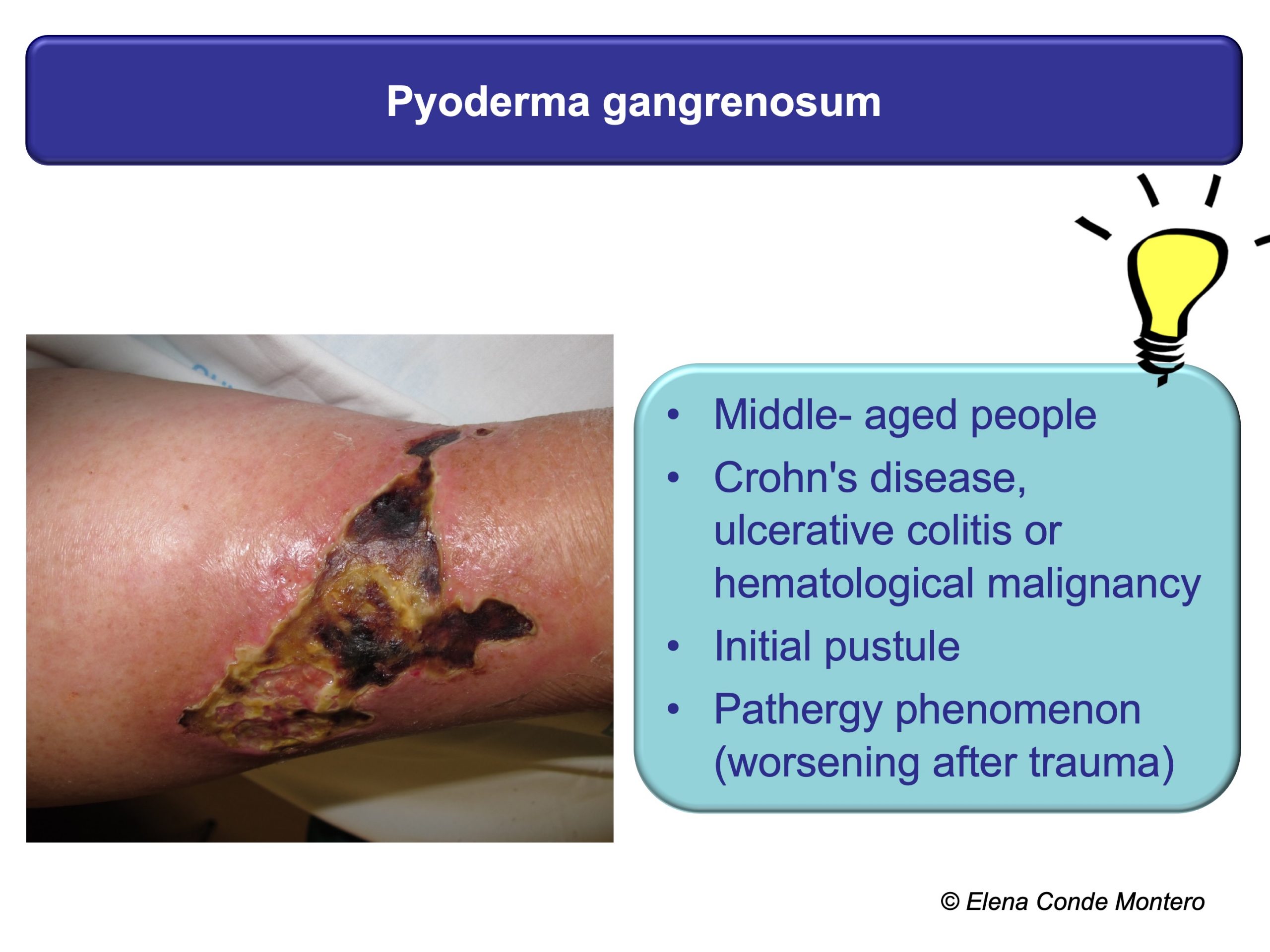
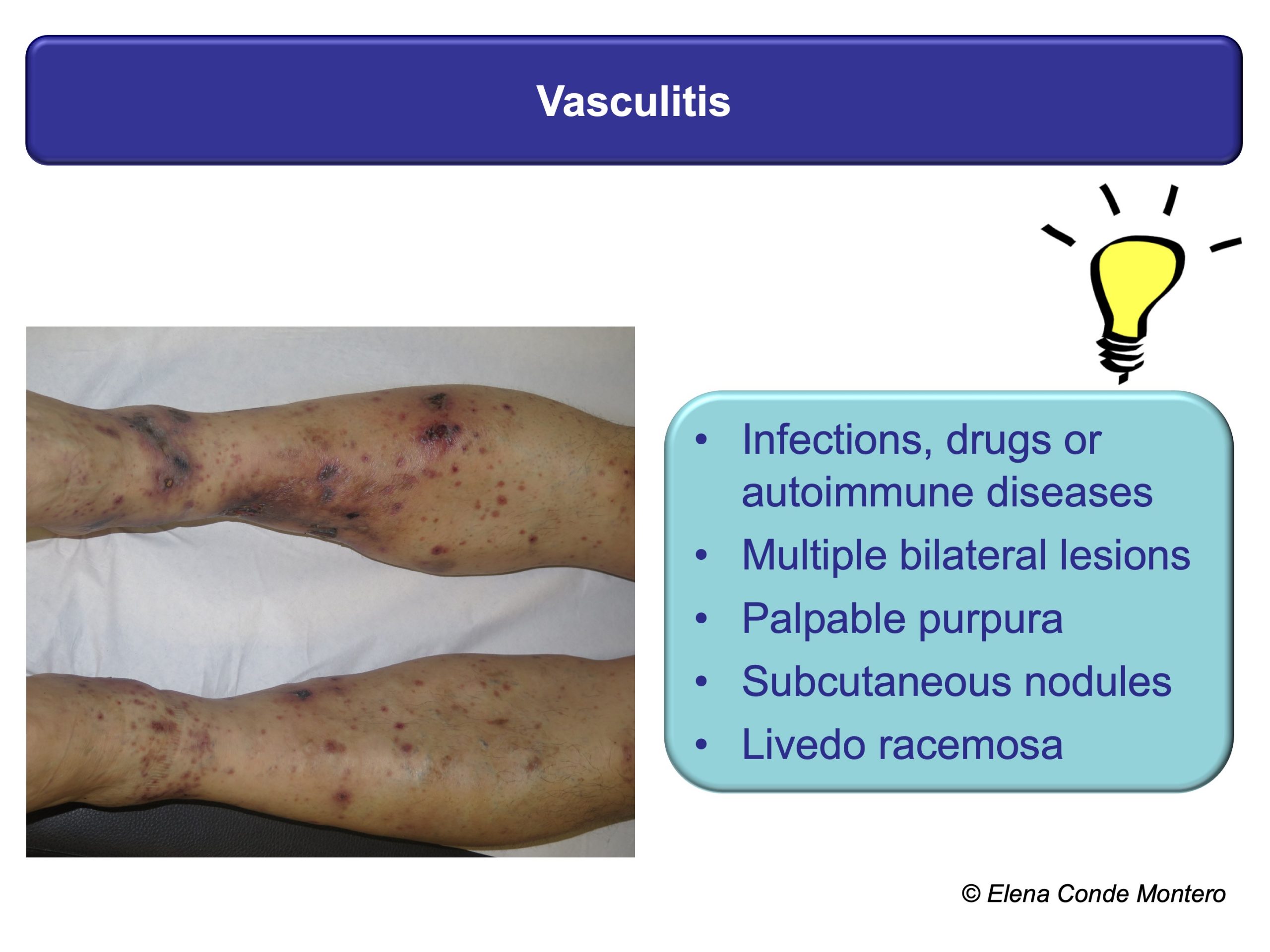
A successful treatment will always be preceded by a proper evaluation of the wound, the leg, the patient and all those factors that may be preventing its healing. This is fundamental because the different pathologies that present with necrotic ulcers may present similar clinical characteristics such as pain, purpuric edges or rapid progression of the lesions, which do not help to differentiate them. This “clinical picture” can be found, among other causes, in pyoderma gangrenosum, calcifilaxia, Martorell ulcer or vasculitis. In addition to these diseases, patients may also present chronic venous insufficiency. It is important to identify it since, although it is not the cause of the wound, it is a reason for greater inflammation and consequent necrosis.

In the EWMA document and in other previous posts you can find a detailed description of these 4 types of wounds (physiopathology, clinical, diagnostic, treatment), but here I propose some clues that can guide your suspicions from the first visit. As you can see, the personal history of the patient, the evolution and location of the ulcers, and other skin signs can be very useful.
These patients have to be referred to the specialist for adequate histological and analytical tests. The skin biopsy can give us a lot of information. It must be taken from the edge of the lesion and must be extensive and deep to see the deep dermis vessels and subcutaneous cellular tissue (better wedge biopsy than punch).


If vasculitis is suspected, in order to detect the most specific inflammation, the biopsy will be performed on the most recent lesion and a sample will also be sent for study with direct immunofluorescence. Although the histological findings in some cases, such as pyoderma gangrenosum, are not specific, the biopsy will help us to support the diagnosis and exclude other causes.
The list of leg wounds with purple edges and necrotic tissue is very broad, and includes from bites or trauma (see post “Large leg wounds after mild leg trauma“) to occlusive vasculopathies with different triggers. An adequate anamnesis is essential, since, for example, in the case of stings or trauma, the conversation with the patient can reveal the cause. In immunosuppressed patients or those who have travelled to tropical countries, we must think about infectious causes, which can also occur with necrosis (such as ecthyma and gangrenous ecthyma) and, in addition to the biopsy for histological examination, a skin sample will be sent for microbiological examination.
As I always say, the important thing is not to know all the possible causes that could justify a wound with necrotic tissue, but to know how to detect clues that can guide the diagnosis or at least make us think that it is not a “typical ulcer” and that it needs a referral to a specialist.
I would like to end with the “trick” that we do very well in our practice, which makes few things scare us: teamwork! ?

Also available in: Español (Spanish)










